J Korean Ophthalmol Soc.
2014 Apr;55(4):555-562.
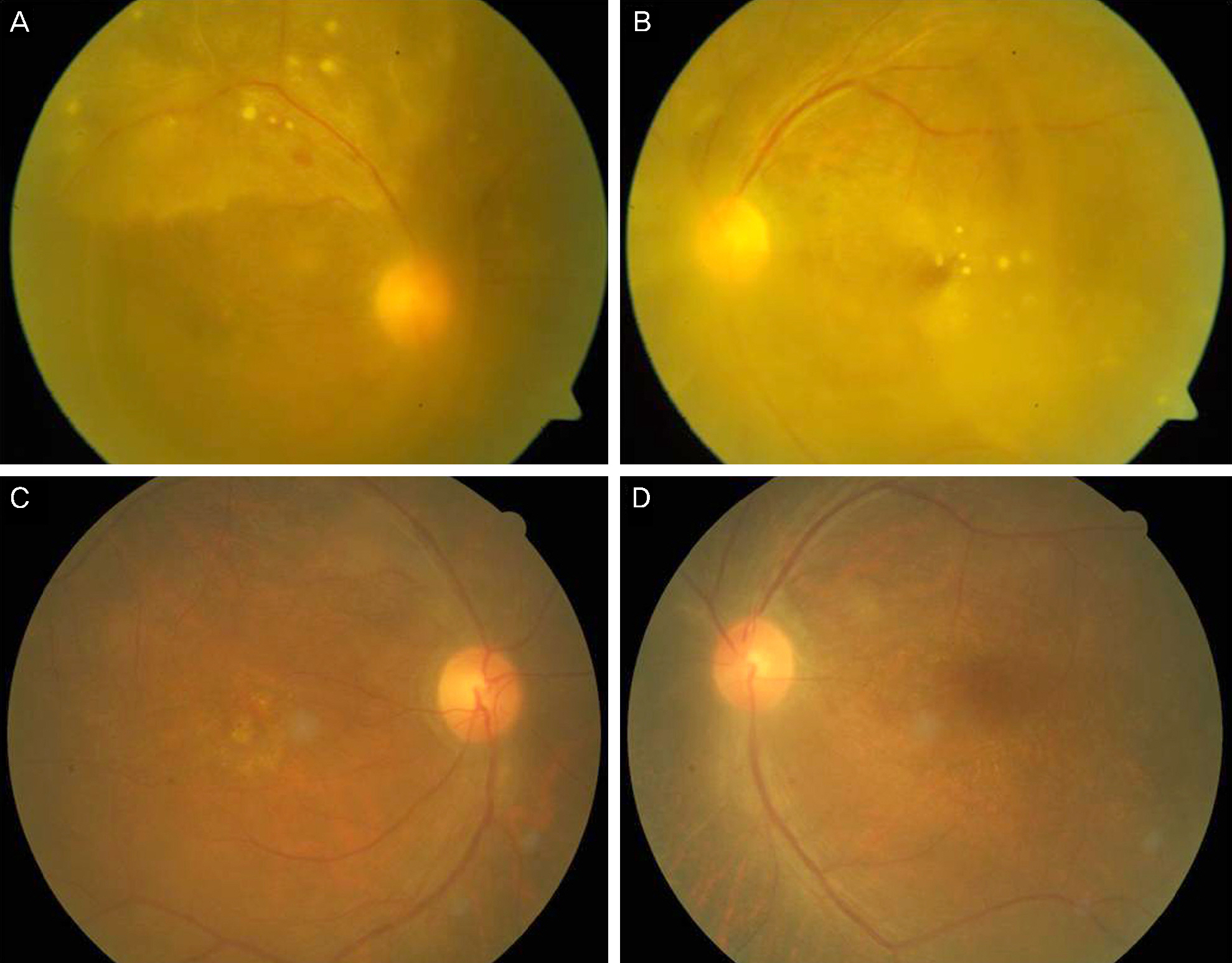
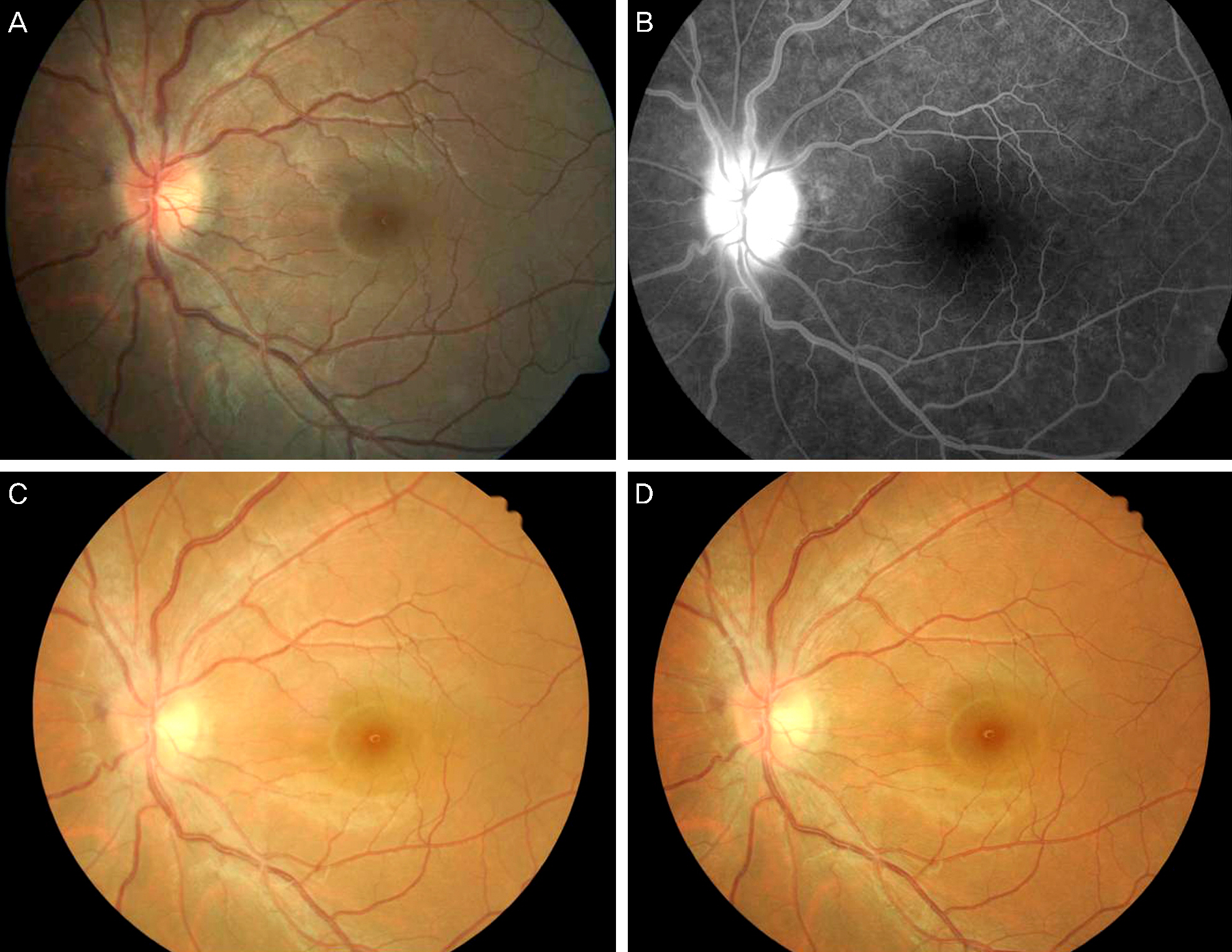
Clinical Manifestations of Syphilitic Uveitis in the Korean Population
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. maekbak@hanmail.net
- 2Department of Ophthalmology, Pusan National University School of Medicine, Busan, Korea.
- 3Department of Ophthalmology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 4Department of Ophthalmology, Kosin University College of Medicine, Busan, Korea.
Abstract
- PURPOSE
In recent, years, an increase of syphilis infections has become an issue in Korea as well as globally. Herein, we report a recent clinical manifestation of syphilitic uveitis in a Korean population.
METHODS
Over a 5-year period (2007-2012), we collected and analyzed the medical records of 16 patients with syphilitic uveitis in three tertiary eye clinics in Pusan. Sixteen patients were confirmed to have syphilis based on serological tests. Retrospective chart review was performed to determine the best corrected visual acuity, anterior and posterior segments, and treatment regimen, as well as ancillary test results including fluorescein angiogram (FAG).
RESULTS
Of the 16 patients, 12 were males and four were females. The mean age of the patients was 51.16 years. Non-granulomatous anterior uveitis was observed in nine eyes (47.4%). Vitritis was the most frequently observed posterior segment finding (16 eyes, 84.2%). Retinal vasculitis and chorioretinitis were found in 11 (57.9%) and five eyes (26.3%), respectively. All patients had negative results in the serum HIV antibody test. Of the 16 patients, 15 were treated with penicillin or ceftriaxone due to neurosyphilis. Mean visual acuity improved from 1.33 +/- 1.1 to 0.58 +/- 0.68 after treatment.
CONCLUSIONS
Clinical manifestation of syphilitic uveitis in Korean patients is different from occurrences in Western countries. Ophthalmological findings of syphilitic uveitis are diverse; thus, serological testing for syphilis is recommended for all uveitis patients. Further research regarding long-term treatment, relapse of syphilitic uveitis, and complications is necessary.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Goldsmith LA, Katz SI, Gilchrest BA, et al. Fitzpatrick's Dermatology in General Medicine. 8th ed.New York: McGraw-Hill;2008. p. 1955–7.2. Primary and secondary syphilis--United States, 2003-2004. MMWR Morb Mortal Wkly Rep. 2006; 55:269–73.3. Herida M, Michel A, Goulet V, et al. Epidemiology of sexually transmitted infections in France. Med Mal Infect. 2005; 35:281–9.4. Parc CE, Chahed S, Patel SV, Salmon-Ceron D. Manifestations and treatment of ocular syphilis during an epidemic in France. Sex Transm Dis. 2007; 34:553–6.
Article5. Anshu A, Cheng CL, Chee SP. Syphilitic uveitis: an Asian perspective. Br J Ophthalmol. 2008; 92:594–7.
Article6. Gaudio PA. Update on ocular syphilis. Curr Opin Ophthalmol. 2006; 17:562–6.
Article7. Baughn RE, Musher DM. Secondary syphilitic lesions. Clin Microbiol Rev. 2005; 18:205–16.
Article8. Singh AE, Romanowski B. Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features. Clin Microbiol Rev. 1999; 12:187–209.
Article9. Foster C. Stephen, Vitale Albert T., Pomerantz , et al. Diagnosis and Treatment of Uveitis. Philadelphia: WB Sounders CO.;2002.10. Barile GR, Flynn TE. Syphilis exposure in patients with uveitis. Ophthalmology. 1997; 104:1605–9.
Article11. Tamesis RR, Foster CS. Ocular syphilis. Ophthalmology. 1990; 97:1281–7.
Article12. Drancourt M, Berger P, Terrada C, et al. High prevalence of fastid-ious bacteria in 1520 cases of uveitis of unknown etiology. Medicine (Baltimore). 2008; 87:167–76.
Article13. Puech C, Gennai S, Pavese P, et al. Ocular manifestations of syphilis: recent cases over a 2.5-year period. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1623–9.
Article14. Baek JO, Jee HJ, KIm TK, et al. Recent trends of syphilis prevalence in normal population in Korea: a single center study in Seoul. Korean J Dermatol. 2011; 49:106–10.15. Marra CM. Syphilis and human immunodeficiency virus: prevention and politics. Arch Neurol. 2004; 61:1505–8.16. Shalaby IA, Dunn JP, Semba RD, Jabs DA. Syphilitic uveitis in human immunodeficiency virus-infected patients. Arch Ophthalmol. 1997; 115:469–73.
Article17. Tran TH, Cassoux N, Bodaghi B, et al. Syphilitic uveitis in patients infected with human immunodeficiency virus. Graefes Arch Clin Exp Ophthalmol. 2005; 243:863–9.
Article18. Becerra LI, Ksiazek SM, Savino PJ, et al. Syphilitic uveitis in human immunodeficiency virus-infected and noninfected patients. Ophthalmology. 1989; 96:1727–30.
Article19. Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990; 97:1288–97.
Article20. Wickremasinghe S, Ling C, Stawell R, et al. Syphilitic punctate in-ner retinitis in immunocompetent gay men. Ophthalmology. 2009; 116:1195–200.
Article21. Mendelsohn AD, Jampol LM. Syphilitic retinitis. A cause of ne-crotizing retinitis. Retina. 1984; 4:221–4.22. Jay CA. Treatment of neurosyphilis. Curr Treat Options Neurol. 2006; 8:185–92.
Article23. Shann S, Wilson J. Treatment of neurosyphilis with ceftriaxone. Sex Transm Infect. 2003; 79:415–6.
Article24. Zhou P, Gu Z, Xu J, et al. A study evaluating ceftriaxone as a treatment agent for primary and secondary syphilis in pregnancy. Sex Transm Dis. 2005; 32:495–8.
Article25. Steele RW. Ceftriaxone therapy of meningitis and serious infections. Am J Med. 1984; 77:50–3.26. Marra CM, Boutin P, McArthur JC, et al. A pilot study evaluating ceftriaxone and penicillin G as treatment agents for neurosyphilis in human immunodeficiency virus-infected individuals. Clin Infect Dis. 2000; 30:540–4.
Article27. Augenbraun M, Workowski K. Ceftriaxone therapy for syphilis: report from the emerging infections network. Clin Infect Dis. 1999; 29:1337–8.
Article28. Dayan L, Ooi C. Syphilis treatment: old and new. Expert Opin Pharmacother. 2005; 6:2271–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Syphilitic Keratoderma Concurrent with Syphilitic Uveitis
- A Case of Syphilitic Uveitis in an Immunocompetent Patient
- Three Cases of Secondary Syphilis with Simultaneous Primary Syphilitic Lesions
- Syphilitic gastritis: a case report
- A case of the human immunodeficiency virus type 1-infected patient presented as a syphilitic papillitis