J Korean Ophthalmol Soc.
2012 Oct;53(10):1378-1384.
Surgical Outcome of Levator Recession for Correction of Upper Eyelid Retraction
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. yswoph@catholic.ac.kr
- 2Catholic St. Mary's Eye Clinic, Seoul, Korea.
Abstract
- PURPOSE
To assess the efficacy of levator recession under local anesthesia to treat upper eyelid retraction.
METHODS
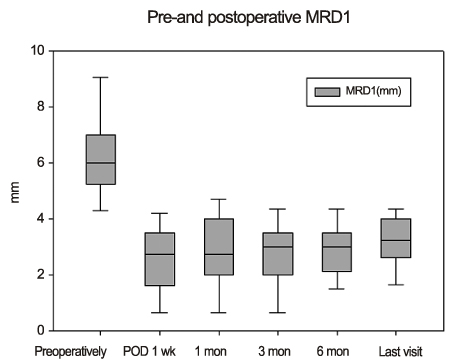
Records of 12 patients (12 lids) were reviewed retrospectively. Postoperative cosmetic results were assessed as good, fair, or poor based on the upper lid height and symmetry. Preoperative and postoperative marginal reflex distance (MRD1, mm), upper eyelid asymmetry, lid lag, lagophthalmos, and ocular exposure symptoms were compared. The reoperation rate was also evaluated.
RESULTS
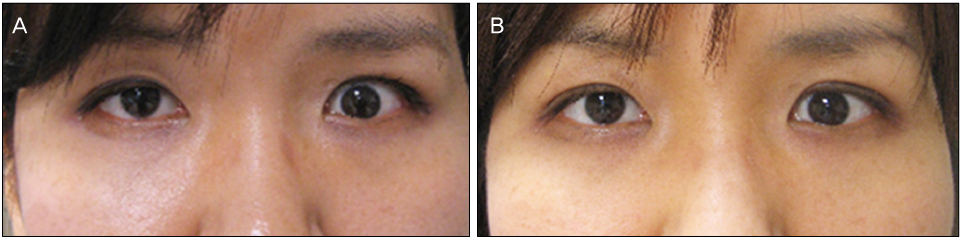
Causes accounting for upper lid retraction were Graves ophthalmopathy (9 lids, 75.0%), orbital pseudotumor (2 lids, 16.7%), and hypercorrection from previous ptosis operation (1 lid, 8.3%). At a mean +/- standard deviation of 27.7 +/- 24.0 months follow-up (range, 5-60 months), 11 patients (91.7%) showed significantly better cosmetic results. MRD1 decreased an average of 3.1 +/- 1.3 mm from 6.3 +/- 1.5 mm preoperatively to 3.2 +/- 0.9 mm postoperatively (p < 0.001). Upper lid asymmetry, lagophthalmos, and lid lag were also reduced significantly (p < 0.001). Overcorrection occurred in 3 lids (25%) and required levator advancement. Eleven patients (91.7%) experienced complete resolution of dry eye symptoms following levator recession.
CONCLUSIONS
Levator recession showed good cosmetic results up to 2 years after surgery for upper eyelid retraction.
MeSH Terms
Figure
Reference
-
1. Clauser L, Galiè M, Sarti E, Dallera V. Rationale of treatment in Graves ophthalmopathy. Plast Reconstr Surg. 2001. 108:1880–1894.2. Kagoshima T, Hori S, Inoue Y. Qualitative and quantitative analyses of Müller's muscle in dysthyroid ophthalmopathy. Jpn J Ophthalmol. 1987. 31:646–654.3. Baldeschi L. Correction of lid retraction and exophthalmos. Dev Ophthalmol. 2008. 41:103–126.4. Baylis HI, Cies WA, Kamin DF. Correction of upper eyelid retraction. Am J Ophthalmol. 1976. 82:790–794.5. Putterman AM, Fett DR. Müller's muscle in the treatment of upper eyelid retraction: a 12-year study. Ophthalmic Surg. 1986. 17:361–367.6. Grove AS Jr. Upper eyelid retraction and Graves' disease. Ophthalmology. 1981. 88:499–506.7. Hedin A. Eyelid surgery in dysthyroid ophthalmopathy. Eye (Lond). 1988. 2(Pt 2):201–206.8. Grove AS Jr. Eyelid retraction treated by levator marginal myotomy. Ophthalmology. 1980. 87:1013–1018.9. Mourits MP, Koornneef L. Lid lengthening by sclera interposition for eyelid retraction in Graves' ophthalmopathy. Br J Ophthalmol. 1991. 75:344–347.10. Elner VM, Hassan AS, Frueh BR. Graded full-thickness anterior blepharotomy for upper eyelid retraction. Arch Ophthalmol. 2004. 122:55–60.11. Thaller VT, Kaden K, Lane CM, Collin JR. Thyroid lid surgery. Eye (Lond). 1987. 1(Pt 5):609–614.12. McNab AA, Galbraith JE, Friebel J, Caesar R. Pre-Whitnall levator recession with hang-back sutures in Graves orbitopathy. Ophthal Plast Reconstr Surg. 2004. 20:301–307.13. Hintschich C, Haritoglou C. Full thickness eyelid transsection (blepharotomy) for upper eyelid lengthening in lid retraction associated with Graves' disease. Br J Ophthalmol. 2005. 89:413–416.14. Lee SH, Lew H, Yun YS. The result of botulinum toxin a injection in the upper eyelid retraction of thyroid-associated ophthalmopathy patients. J Korean Ophthalmol Soc. 2006. 47:1197–1203.15. Lee JY. A statistical study on the corneal diameters in Korean. J Korean Ophthalmol Soc. 1983. 1:53–58.16. Linberg JV, Vasquez RJ, Chao GM. Aponeurotic ptosis repair under local anesthesia. Prediction of results from operative lid height. Ophthalmology. 1988. 95:1046–1052.17. Lee MJ, Oh JY, Choung HK, et al. Frontalis sling operation using silicone rod compared with preserved fascia lata for congenital ptosis a three-year follow-up study. Ophthalmology. 2009. 116:123–129.18. Small RG. Surgery for upper eyelid retraction, three techniques. Trans Am Ophthalmol Soc. 1995. 93:353–365.19. Ceisler EJ, Bilyk JR, Rubin PA, et al. Results of Müllerotomy and levator aponeurosis transposition for the correction of upper eyelid retraction in Graves disease. Ophthalmology. 1995. 102:483–492.20. Tucker SM, Collin R. Repair of upper eyelid retraction: a comparison between adjustable and non-adjustable sutures. Br J Ophthalmol. 1995. 79:658–660.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Levator Recession for Upper Eyelid Retraction in Patients with Thyroid-associated Ophthalmopathy
- Surgical Treatment of Thyroid-related Upper Eyelid Retraction
- Upper Eyelid Retraction Repaired Without Using Spacer
- Staged Correction of Cicatricial Upper Eyelid Retraction and Contralateral Upper Eyelid Ptosis
- Surgical Efficacyin the Upper and Lower Eyelid Retraction