J Korean Ophthalmol Soc.
2012 May;53(5):632-638.
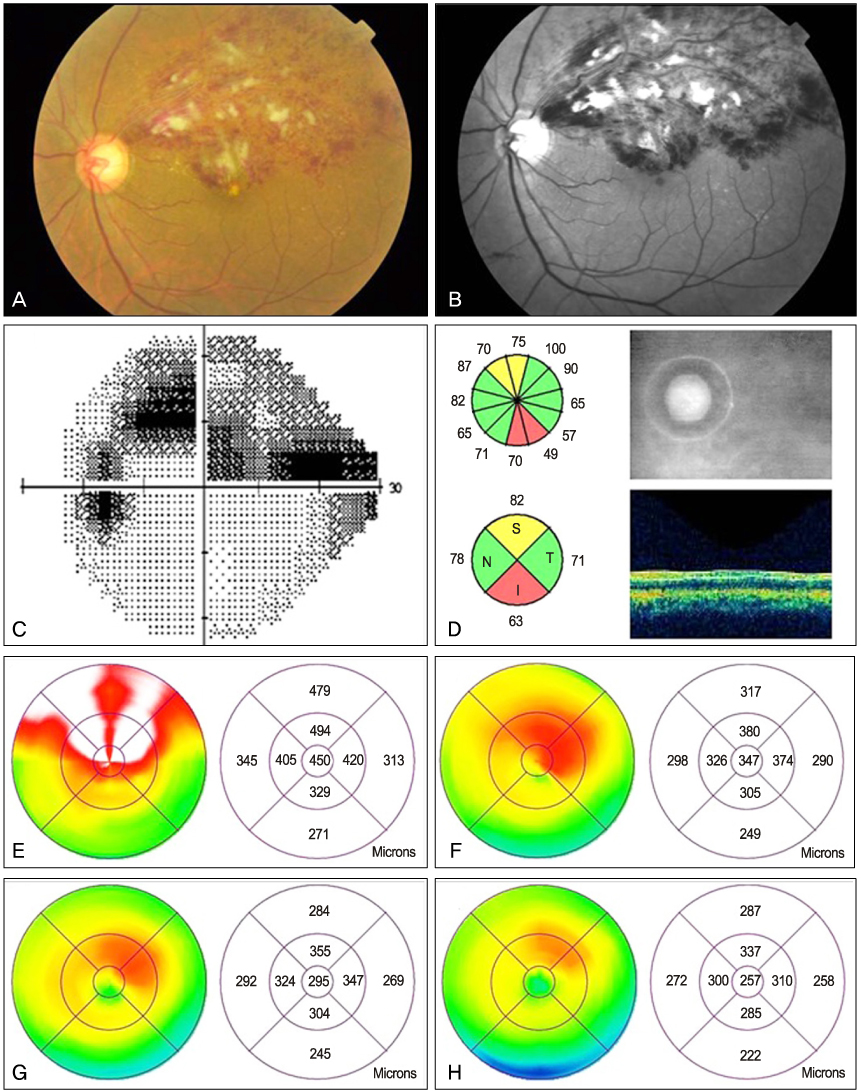
Bevacizumab Therapy for Branch Retinal Vein Occlusion Associated with Normal Tension Glaucoma
- Affiliations
-
- 1Department of Ophthalmology, Happyeye21 Clinic, Gwangju, Korea.
- 2Department of Ophthalmology, Kangdong Sacred Heart Hospital Hallym University College of Medicine, Seoul, Korea. sungpyo@hanafos.com
Abstract
- PURPOSE
To evaluate the therapeutic efficacy of intravitreal bevacizumab (IVB) in the treatment of branch retinal vein occlusion (BRVO) in eyes with normal tension glaucoma (NTG).
METHODS
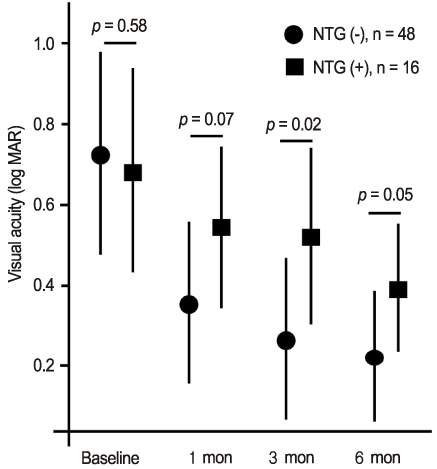
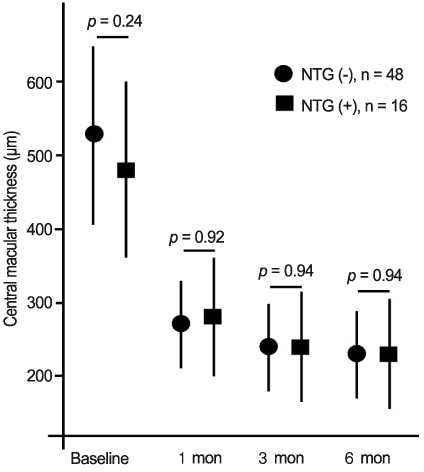
We included 16 NTG eyes and 48 age- and sex-matched eyes without NTG that had received IVB for BRVO with more than 6 months of follow-up. The main outcome measures were log MAR best-corrected visual acuity (BCVA) and central macular thickness (CMT) at baseline and 1, 3, and 6 months after IVB. We compared the results according to the comorbidity associated with NTG.
RESULTS
The obstruction site of BRVO was significantly closer to the optic disc in eyes with NTG than in eyes without NTG. Baseline log MAR BCVA and CMT were similar between the two groups. After IVB, postoperative BCVA was significantly improved and CMT was significantly reduced, irrespective of the comorbidity associated with NTG. However, vision improvement was more limited in eyes with NTG, while CMT was similarly reduced compared with that in eyes without NTG. The mean numbers of injections were similar between the two groups, and there were no injection-related complications.
CONCLUSIONS
IVB may have therapeutic efficacy in the treatment of BRVO associated with NTG. However, the comorbidity associated with NTG may limit vision improvement, although anatomic recovery of CMT is achieved.
Keyword
MeSH Terms
Figure
Reference
-
1. Phillips S, Fekrat S, Finkelstein D. Ryan SJ, editor. Branch retinal vein occlusion. Retina. 2006. v. 2:4th ed. Philadelphia: Mosby;1349–1354.2. Beaumont PE, Kang HK. Cup-to-disc ratio, intraocular pressure, and primary open-angle glaucoma in retinal venous occlusion. Ophthalmology. 2002. 109:282–286.3. Klein BE, Meuer SM, Knudtson MD, Klein R. The relationship of optic disk cupping to retinal vein occlusion: the Beaver Dam Eye Study. Am J Ophthalmol. 2006. 141:859–862.4. Rath EZ, Frank RN, Shin DH, Kim C. Risk factors for retinal vein occlusions. A case-control study. Ophthalmology. 1992. 99:509–514.5. Grieshaber MC, Mozaffarieh M, Flammer J. What is the link between vascular dysregulation and glaucoma? Surv Ophthalmol. 2007. 52:Suppl 2. S144–S154.6. Kim SJ, Park KH. Four cases of normal-tension glaucoma with disk hemorrhage combined with branch retinal vein occlusion in the contralateral eye. Am J Ophthalmol. 2004. 137:357–359.7. Sonnsjö B, Dokmo Y, Krakau T. Disc haemorrhages, precursors of open angle glaucoma. Prog Retin Eye Res. 2002. 21:35–56.8. The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol. 1984. 98:271–282.9. Park SP, Ahn JK. Changes of aqueous vascular endothelial growth factor and interleukin-6 after intravitreal triamcinolone for branch retinal vein occlusion. Clin Experiment Ophthalmol. 2008. 36:831–835.10. Lee H, Shah GK. Intravitreal triamcinolone as primary treatment of cystoid macular edema secondary to branch retinal vein occlusion. Retina. 2005. 25:551–555.11. Rabena MD, Pieramici DJ, Castellarin AA, et al. Intravitreal bevacizumab (Avastin) in the treatment of macular edema secondary to branch retinal vein occlusion. Retina. 2007. 27:419–425.12. Park SP, Ahn JK. Changes of aqueous vascular endothelial growth factor and pigment epithelium-derived factor following intravitreal bevacizumab for macular oedema secondary to branch retinal vein occlusion. Clin Experiment Ophthalmol. 2009. 37:490–495.13. Wu L, Arevalo JF, Roca JA, et al. Comparison of two doses of intravitreal bevacizumab (Avastin) for treatment of macular edema secondary to branch retinal vein occlusion: results from the Pan-American Collaborative Retina Study Group at 6 months of follow-up. Retina. 2008. 28:212–219.14. Lindblom B. Open angle glaucoma and non-central retinal vein occlusion--the chicken or the egg? Acta Ophthalmol Scand. 1998. 76:329–333.15. Flammer J, Orgül S, Costa VP, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002. 21:359–393.16. Flammer J, Pache M, Resink T. Vasospasm, its role in the pathogenesis of diseases with particular reference to the eye. Prog Retin Eye Res. 2001. 20:319–349.17. Park SP, Ahn JK, Mun GH. Aqueous vascular endothelial growth factor levels are associated with serous macular detachment secondary to branch retinal vein occlusion. Retina. 2010. 30:281–286.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Analysis of the Hemispheric Retinal Vein Occlusion
- Neovascular Glaucoma Due to Branch Retinal Vein Occlusion Combined with Branch Retinal Artery Occlusion
- Two Cases of Macular Edema Associated with Extramacular Branch Retinal Vein Occlusion
- A Clinical Study on the Occlusion of the Retinal Vein
- Clinical observation of the bilateral branch vein occlusion