J Korean Ophthalmol Soc.
2011 Apr;52(4):487-491.
The Recurrent Submacular Hemorrhage after Removal of Sub-Internal Limiting Membrane Hemorrhage with Retinal Arterial Macroaneurysm
- Affiliations
-
- 1Department of Ophthalmology, Chungnam National University College of Medicine, Daejeon, Korea. youngjoon@cnu.ac.kr
- 2Institute for Medical Sciences, Chungnam National University Research, Daejeon, Korea.
Abstract
- PURPOSE
To report a case of a recurrent macular hemorrhage that developed after surgical removal of the internal limiting membrane (ILM) for subintimal hemorrhage due to retinal macroaneurysm.
CASE SUMMARY
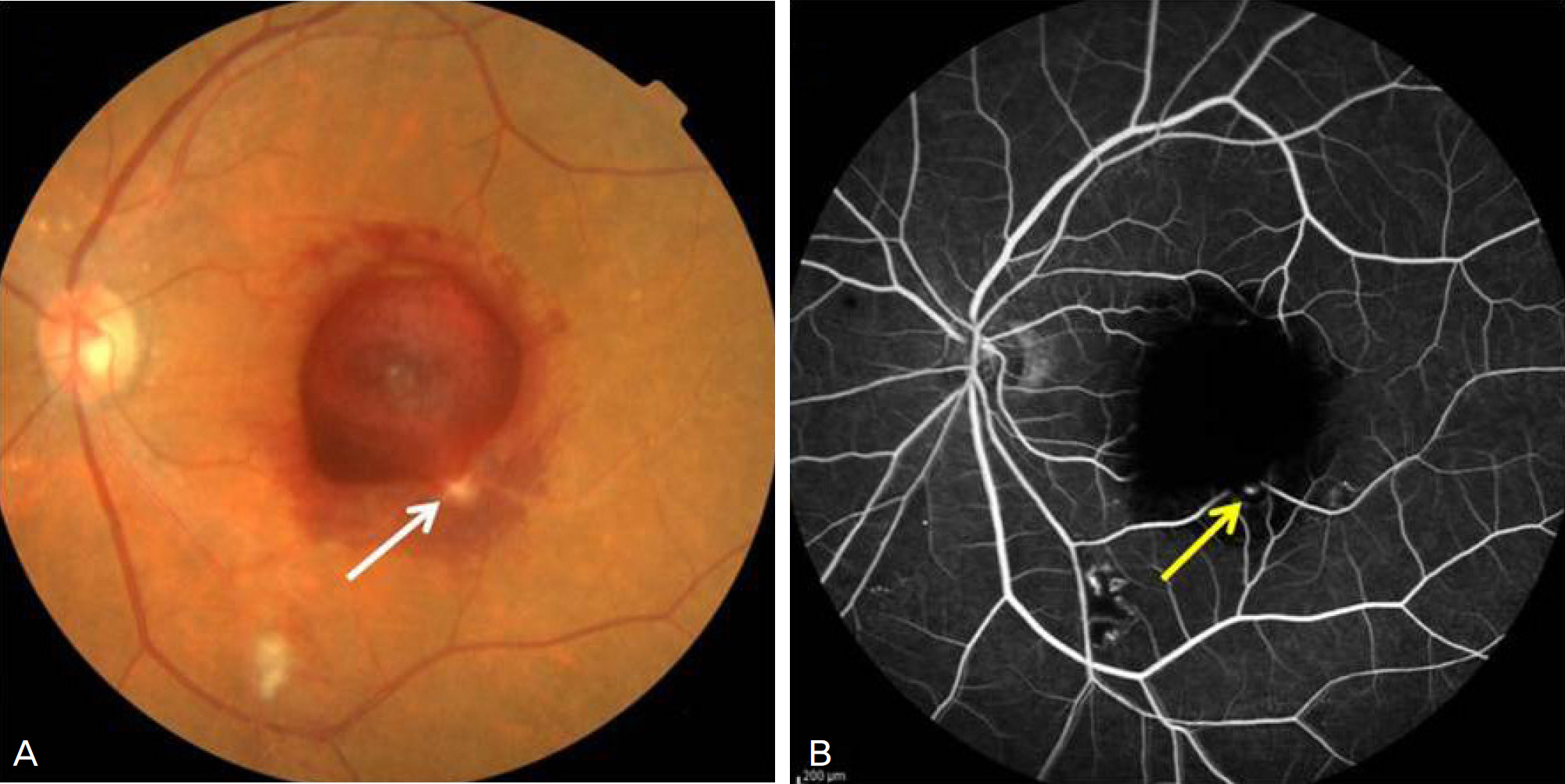
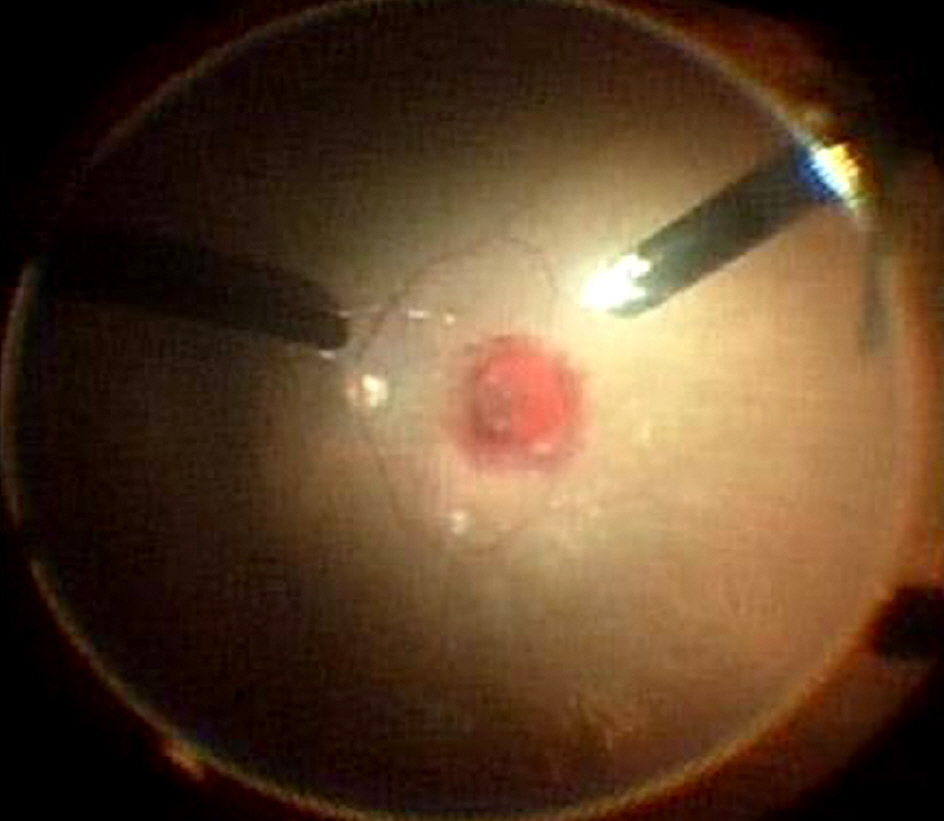
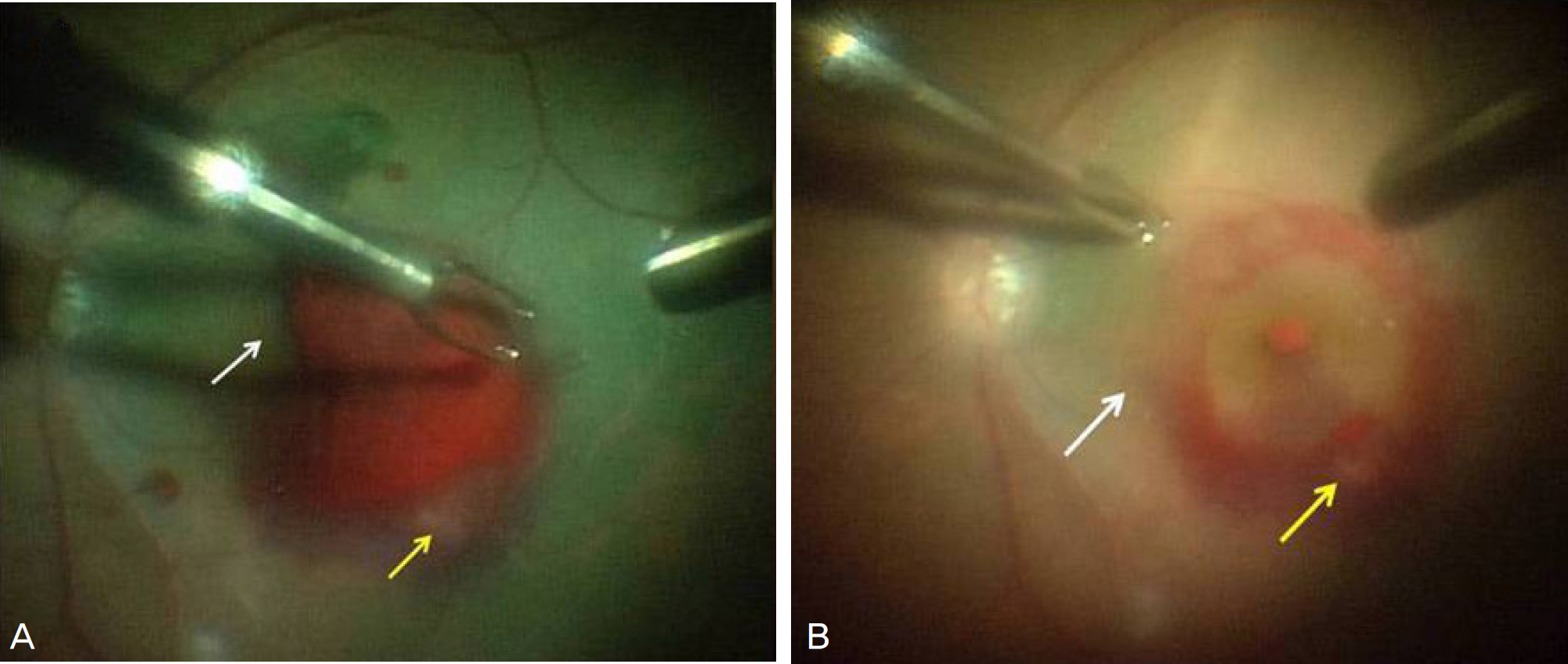
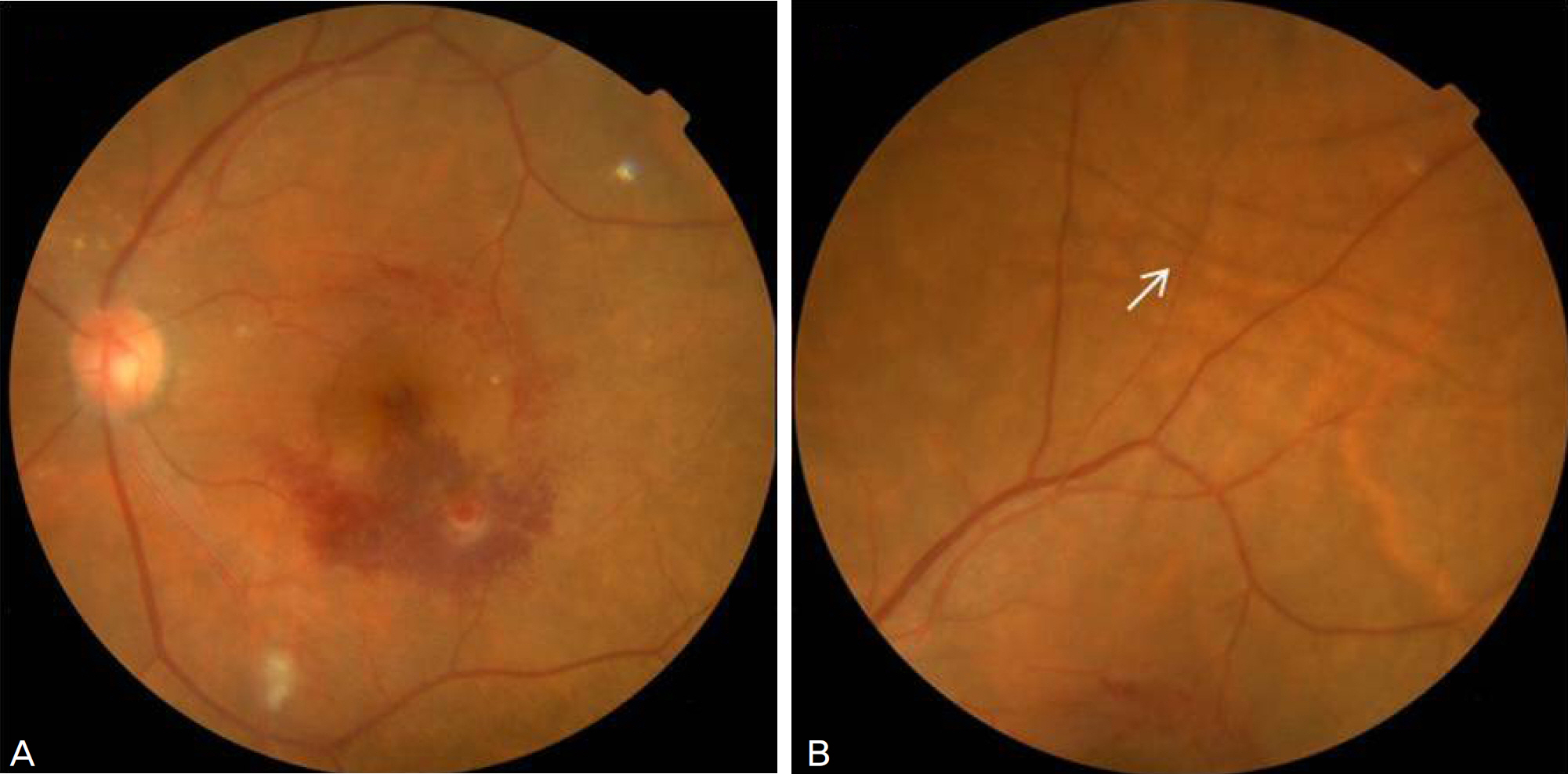
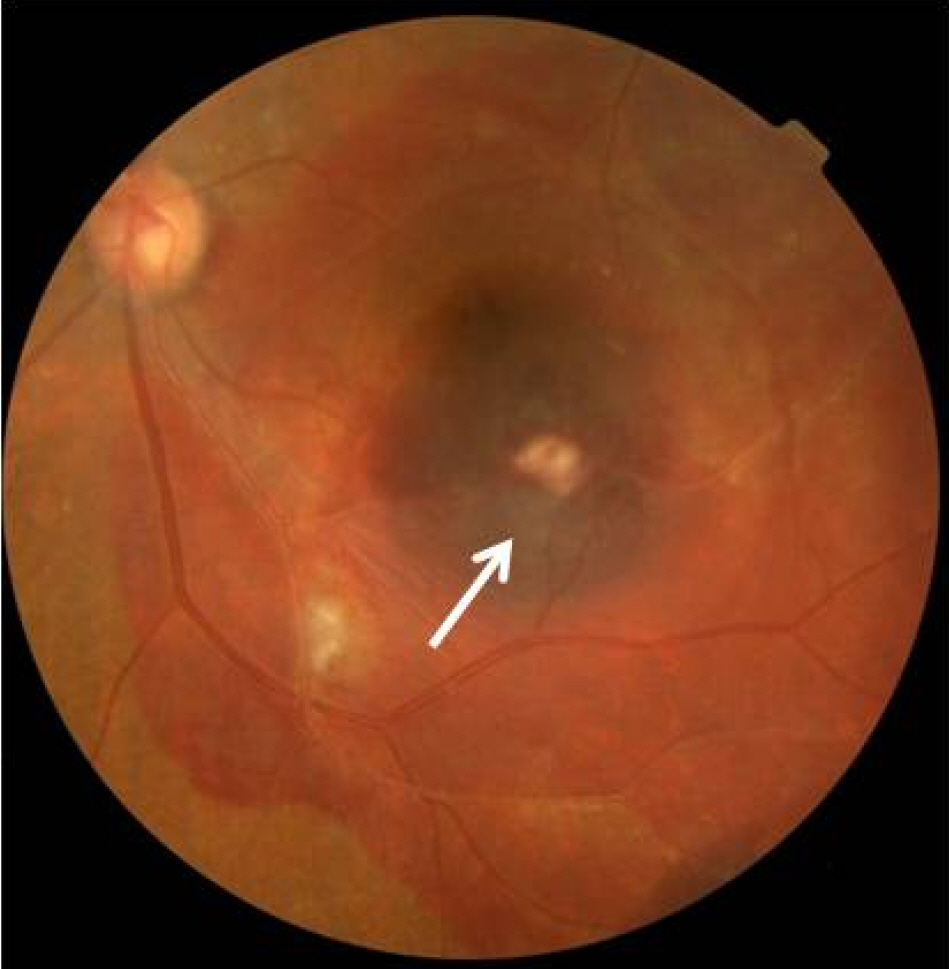
A 75-year-old female was admitted to the hospital complaining of decreased vision in the left eye which had started 3 weeks previously. The best corrected visual acuity (BCVA) of the right and left eye was 0.7 and 0.03, respectively. The intraocular pressure (IOP) of the right and left eye was 10 mm Hg and 12 mm Hg, respectively. On the fundus examination, macular preretinal and subretinal hemorrhage was observed and a diagnosis of retinal arterial macroaneurym of the inferonasal major artery was made. Vitrectomy was performed. After indocyanine green dye staining, the sub-ILM hemorrhage was treated with removal of the ILM. At postoperative day 3, the annular chorioretinal folds were observed due to the hypotony (4 mm Hg). However, the absence of leakage was confirmed through the sclerotomy site. At postoperative day 8, recurrent submacular hemorrhage occurred and the hemorrhage was observed to have spread after intravitreal C3F8 gas injection and when the patient was placed in the prone position. At postoperative 4 months, the hemorrhage that had invaded the macular area was completely resolved. The BCVA was 0.3, respectively.
CONCLUSIONS
When removing a sub-ILM hemorrhage due to retinal macroaneurysm, recurrent hemorrhage can occur especially in a patient with ocular hypotony, as in the present case report. Physicians should be aware of this possibility and the proper treatment the condition requires.
Keyword
MeSH Terms
Figure
Reference
-
References
1. McCabe CM, Flynn HW Jr, McLean WC, et al. Nonsurgical management of macular hemorrhage secondary to retinal artery macroaneurysms. Arch Ophthalmol. 2000; 118:780–5.
Article2. Zhao P, Hayashi H, Oshima K, et al. Vitrectomy for macular hemorrhage associated with retinal arterial macroaneurysm. Ophthalmology. 2000; 107:613–7.
Article3. Rabb MF, Gagliano DA, Teske MP. Retinal arterial macroaneurysms. Surv Ophthalmol. 1988; 33:73–96.
Article4. Abdel-Khalek MN, Richardson J. Retinal macroaneurysm: natural history and guidelines for treatment. Br J Ophthalmol. 1986; 70:2–11.
Article5. Palestine AG, Robertson DM, Goldstein BG. Macroaneurysms of the retinal arteries. Am J Ophthalmol. 1982; 93:164–71.
Article6. Hotta K, Hotta J. Case of recurrent macular haemorrhage after removal of a sub-internal limiting membrane haematoma secondary to retinal artery macroaneurysm. Clin Experiment Ophthalmol. 2006; 34:610–2.
Article7. Sony P, Gupta V, Sihota R. Macular hole and sub-hyaloid hemorrhage following filtering surgery with mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2005; 243:840–2.
Article8. Fechtner RD, Minckler D, Weinreb RN, et al. Complications of glaucoma surgery. Ocular decompression retinopathy. Arch Ophthalmol. 1992; 110:965–8.9. Rodrigues EB, Costa EF, Penha FM, et al. The use of vital dyes in ocular surgery. Surv Ophthalmol. 2009; 54:576–617.
Article10. Iwase T, Jo YJ, Tanaka N. Ocular hypotony after the use of indocyanine green for epiretinal membrane surgery. Cutan Ocul Toxicol. 2010; 29:130–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Natural Visual Outcome of Submacular Hemorrhage Associated with Retinal Arterial Macroaneurysm
- Bevacizumab Monotherapy for Macular Hemorrhage Secondary to a Retinal Arterial Macroaneurysm
- Full Thickness Macular Hole formation following Rupture of Retinal Arterial Macoraneur
- Treatment of Retinal Arterial Macroaneurysm
- Ruptured Retinal Arterial Macroaneurysm after Panretinal Photocoagulation for Diabetic Retinopathy