J Korean Ophthalmol Soc.
2010 Dec;51(12):1579-1583.
Clinical Features of Nevus of Ota in Korean Population
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea. eyeminerva@yahoo.co.kr
- 2Department of Ophthalmology, Seoul National University Boramae Hospital, Seoul, Korea.
- 3Department of Ophthalmology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
Abstract
- PURPOSE
To investigate the clinical features of the nevus of Ota in the Korean population.
METHODS
A retrospective chart review of the medical records from 94 patients (100 eyes), diagnosed to have a nevus of Ota from September 2005 to February 2010, was performed.
RESULTS
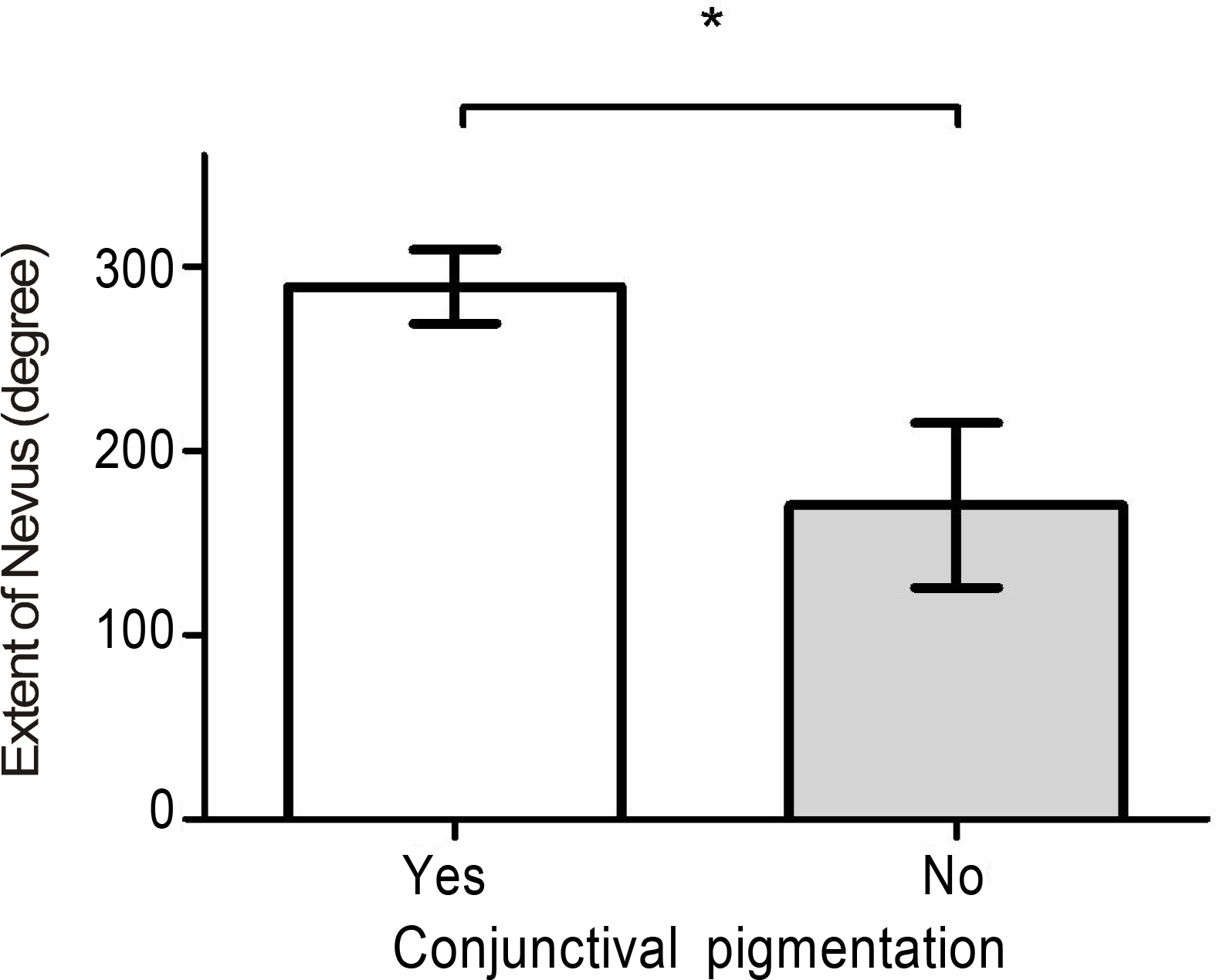
The mean age of detection of a nevus of Ota was 8 months, and the mean extent of the nevus was 253 degrees, which covered more than 2 quadrants in most cases. The patients with a faint nevus tended to be younger. Pigmentation did not reach the fornix, but the limbus was mostly pigmented. Combined conjunctival pigmentation was observed in 61.7% of cases. The pigmentation was significantly associated with a greater extent of the nevus. Iris pigmentation was demonstrated in 98.7% of cases.
CONCLUSIONS
The clinical features of nevi of Ota were diverse regarding the location, extent, and color of the lesion. Conjunctival pigmentation was associated with the extent of the nevus. Iris pigmentation was revealed in almost all cases; therefore, this feature had the diagnostic value for a nevus of Ota. Young patients with a nevus of Ota may mimic osteogenesis imperfecta, which necessitates careful consideration upon differential diagnosis.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Gupta GP, Gangwar DN. Naevus of Ota. Br J Ophthalmol. 1965; 49:364–8.
Article2. Cho KY, Eun HC, Lee YS. Clinical aspects of nevus of Ota and ex-tracutaneous pigmentation. Korean J Dermatol. 1986; 24:67–71.3. Teekhasaenee C, Ritch R, Rutnin U, Leelawongs N. Ocular findings in oculodermal melanocytosis. Arch Ophthalmol. 1990; 108:1114–20.
Article4. Al-Sadhan Y, Shawaf S, Tabbara K. Oculodermal melanosis with choroidal melanoma in a black patient: a case report. Eye (Lond). 2006; 20:1437–8.
Article5. Qian Y, Zakov ZN, Schoenfield L. Iris melanoma arising in iris nevus in oculo (dermal) melanocytosis. Surv Ophthalmol. 2008; 53:411–5.6. Teekhasaenee C, Ritch R, Rutnin U, et al. Glaucoma in oculodermal melanocytosis. Ophthalmology. 1990; 97:562–70.
Article7. Araie M. Oculodermal melanocytosis. J Glaucoma. 2002; 11:454–7.
Article8. Yoon JT, Tchah HW. The surgical treatment of nevus of Ota with ocular involvement. J Korean Ophthalmol Soc. 1999; 40:3229–33.9. Cho BJ, Han YG, Kim JH, et al. Cosmetic repair of nevus of Ota. J Korean Ophthalmol Soc. 2006; 47:996–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Bilateral Nevus of Ota Associated with Bilateral Nevus of Ito
- A Case of Ota Nevus Associated with Altitudinal Field Defect
- A Case of Bilateral Nevus of Ota Associated with Nevus of Ito
- Retrospective Study on the Clinical Features of Ota's Nevus
- Tree Cases of Aquired bilateral Nevus of Ota-like Marcules