J Korean Ophthalmol Soc.
2010 Aug;51(8):1054-1063.
Comparison of Outcomes of Femtosecond Laser-assisted Keratoplasty and Conventional Penetrating Keratoplasty
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea School of Medicine, Seoul, Korea. ckjoo@catholic.ac.kr
- 2Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3The Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
To compare the outcomes of IntraLase femtosecond laser-enabled keratoplasty (IEK) versus conventional penetrating keratoplasty (C-PKP).
METHODS
This retrospective study included 18 eyes of 17 patients who underwent C-PKP and 26 eyes of 25 patients who underwent IEK. Postoperative clinical results were compared between two groups.
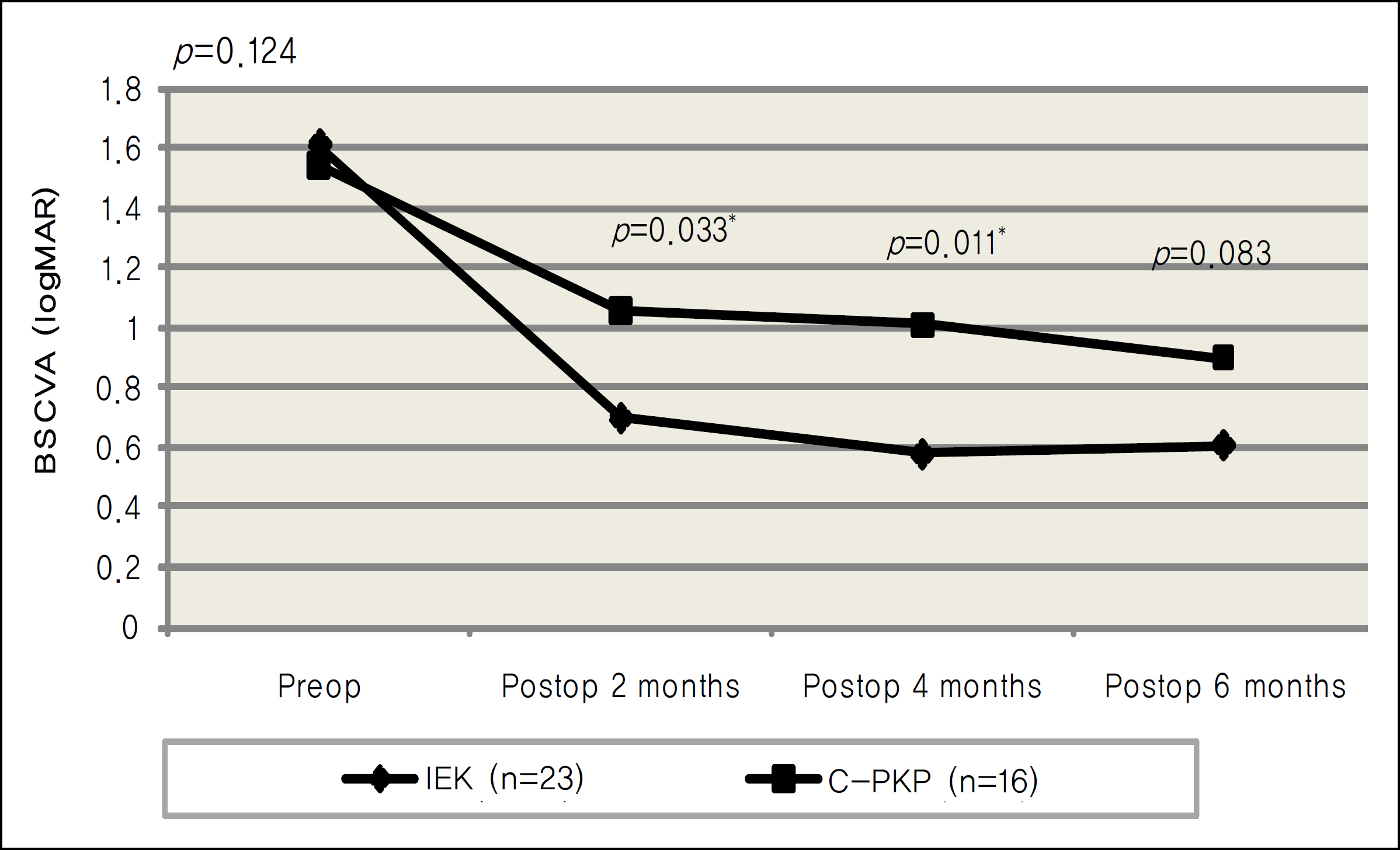
RESULTS
The mean logMAR best spectacle-corrected visual acuity (BSCVA) was 0.70, 0.58, and 0.61 in the IEK group, and 1.06, 1.01, and 0.90 in the C-PKP group at postoperative 2, 4, and 6 months respectively. The difference between the two groups was statistically significant at 2 and 4 months postoperatively (p=0.033, 0.011). The mean refractive cylinder was 4.08 diopters (D), 4.01D, and 4.44D in the IEK group, while 5.75D, 5.75D, and 5.21D in the C-PKP group for each month, and the difference between the groups was statistically significant at 2 and 4 months postoperatively (p=0.037, 0.027). The complication rate showed no significant differences up to 6 months of follow-up between the two groups.
CONCLUSIONS
The IEK showed better results in BSCVA and refractive astigmatism in the early postoperative period, in comparison with the C-PKP, and can be considered as a valuable method in penetrating keratoplasty.
MeSH Terms
Figure
Reference
-
References
1. Ing JJ, Ing HH, Nelson LR, et al. Ten-year postoperative results of penetrating keratoplasty. Ophthalmology. 1998; 105:1855–65.
Article2. Thompson RW Jr, Price MO, Bowers PJ, Price FW Jr. Long-term graft survival after penetrating keratoplasty. Ophthalmology. 2003; 110:1396–402.
Article3. Kaiserman I, Bahar I, Rootman DS. Corneal wound malapposition after penetrating keratoplasty: an optical coherence tomography study. Br J Ophthalmol. 2008; 92:1103–7.
Article4. Farid M, Kim M, Steinert RF. Results of penetrating keratoplasty performed with a femtosecond Laser zigzag incision initial report. Ophthalmology. 2007; 114:2208–12.
Article5. Ignacio TS, Nguyen TB, Chuck RS, et al. Top hat wound configuration for penetrating keratoplasty using the femtosecond laser: a laboratory model. Cornea. 2006; 25:336–40.6. Frost NA, Wu J, Lai TF, Coster DJ. A review of randomized controlled trials of penetrating keratoplasty techniques. Ophthalmology. 2006; 113:942–9.
Article7. Barraquer JI Jr. Technique of penetrating keratoplasty. Am J Ophthalmol. 1950; 33:6–17.
Article8. Binder PS, Abel R Jr, Polack FM, Kaufman HE. Keratoplasty wound separations. Am J Ophthalmol. 1975; 80:109–15.
Article9. Farley MK, Pettit TH. Traumatic wound dehiscence after penetrating keratoplasty. Am J Ophthalmol. 1987; 104:44–9.
Article10. Rehany U, Rumelt S. Ocular trauma following penetrating keratoplasty: incidence, outcome, and postoperative recommendations. Arch Ophthalmol. 1998; 116:1282–6.11. Tseng SH, Lin SC, Chen FK. Traumatic wound dehiscence after penetrating keratoplasty: clinical features and outcome in 21 cases. Cornea. 1999; 18:553–8.12. Melles GR, Lander F, van Dooren BT, et al. Preliminary clinical results of posterior lamellar keratoplasty through a sclerocorneal pocket incision. Ophthalmology. 2000; 107:1850–6.13. Alio JL, Shah S, Barraquer C, et al. New techniques in lamellar keratoplasty. Curr Opin Ophthalmol. 2002; 13:224–9.
Article14. Mearza AA, Qureshi MA, Rostron CK. Experience and 12-month results of Descemet-stripping endothelial keratoplasty (DSEK) with a small-incision technique. Cornea. 2007; 26:279–83.
Article15. Busin M. A new lamellar wound configuration for penetrating keratoplasty surgery. Arch Ophthalmol. 2003; 121:260–5.
Article16. Malta JB, Soong HK, Shtein R, et al. Femtosecond Laser-assisted keratoplasty: laboratory studies in eye bank eyes. Curr Eyes Res. 2009; 34:18–25.
Article17. Stern D, Schoenlein RW, Puliafito CA, et al. Corneal ablation by nanosecond, picosecond, and femtosecond lasers at 532 and 625 nm. Arch Ophthalmol. 1989; 107:587–92.
Article18. Bahar I, Kaiserman I, McAllum P, Rootman D. Femtosecond laser-assisted penetrating keratoplasty stability evaluation of different wound configurations. Cornea. 2008; 27:209–11.19. Price FW, Price MO. Adult keratoplasty: has the prognosis improved in the last 25 years? Int Ophthalmol. 2008; 28:141–6.20. Bahar I, Kaiserman I, Lange AP, et al. Femtosecond laser versus manual dissection for top hat penetrating keratoplasty. Br J Oophthalmol. 2009; 93:73–8.
Article21. Claesson M, Armitage WJ. Astigmatism and the impact of relaxing incisions after penetrating keratoplasty. J Refract Surg. 2007; 23:284–9.
Article22. Sohn BJ, Kim HK. Early results of Femtosecond laser-assisted mushroom-shaped wound-configurized keratoplasty. J Korean Ophthalmol Soc. 2009; 50:34–43.
Article23. Price FW Jr., Price MO, Jordan CS. Safety of incomplete incision patterns in femtosecond laser-assisted penetrating keratoplasty. J Cataract Refract Surg. 2008; 34:2099–103.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Long-term Clinical Outcomes of Penetrating Keratoplasty Using a Manual Trephine and Femtosecond-Laser Trephination
- A Case Report of Fungal Keratitis Diagnosed by Femtosecond Laser Assisted Corneal Biopsy
- Early Results of Femtosecond Laser-Assisted Mushroom-Shaped Wound-Configurized Keratoplasty
- Early Result of Femtosecond Laser Assisted Descemet's Membrane Stripping Endothelial Keratoplasty
- Cataract Extraction after Penetrating Keratoplasty