J Korean Ophthalmol Soc.
2008 Oct;49(10):1690-1695.
A Case Report of Intractable Scleritis Effectively Treated with Infliximab
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. kmk9@snu.ac.kr
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- 3Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
Abstract
- PURPOSE
To report a case of a patient with intractable scleritis with conventional immunosuppressive therapy who showed effective treatment with infliximab.
CASE SUMMARY
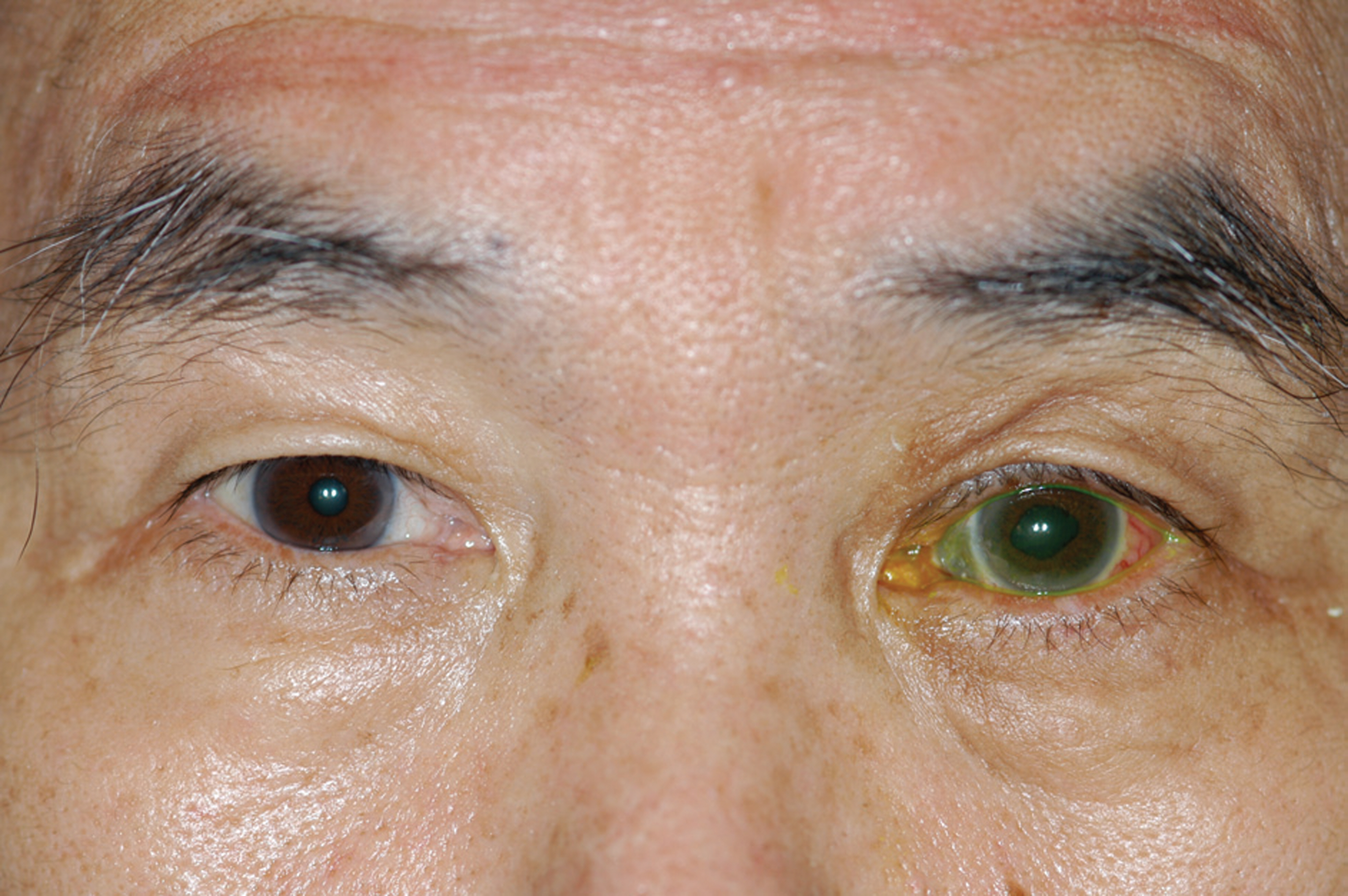
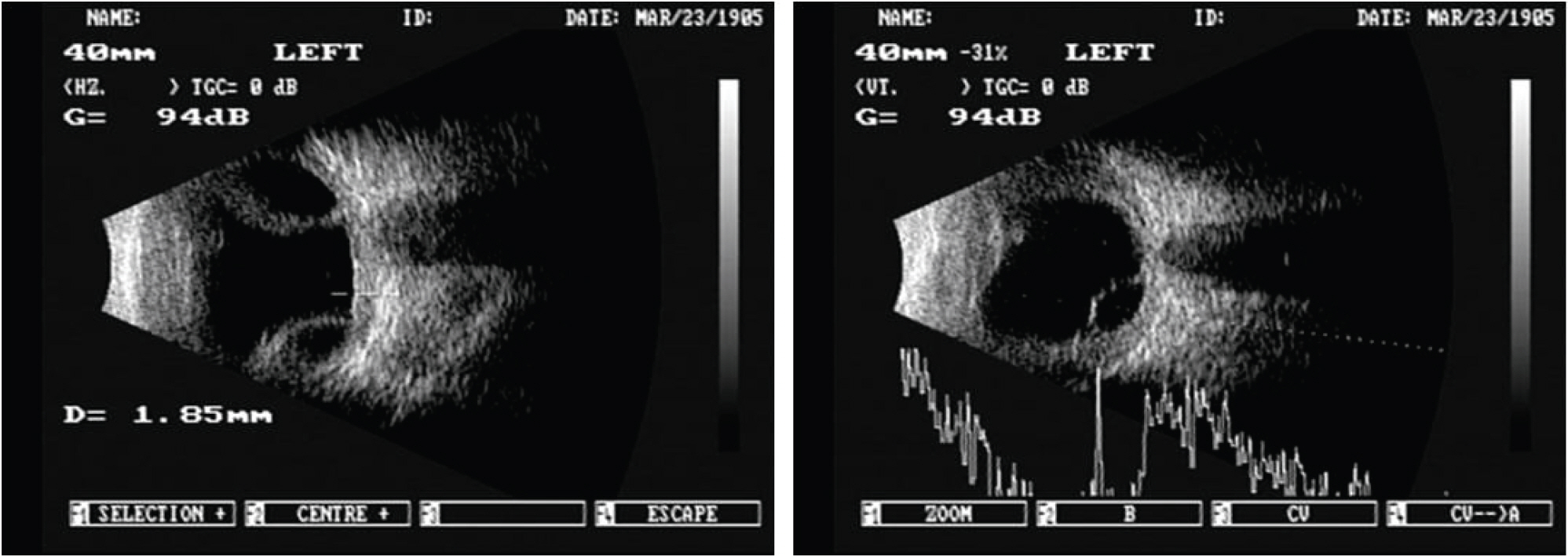
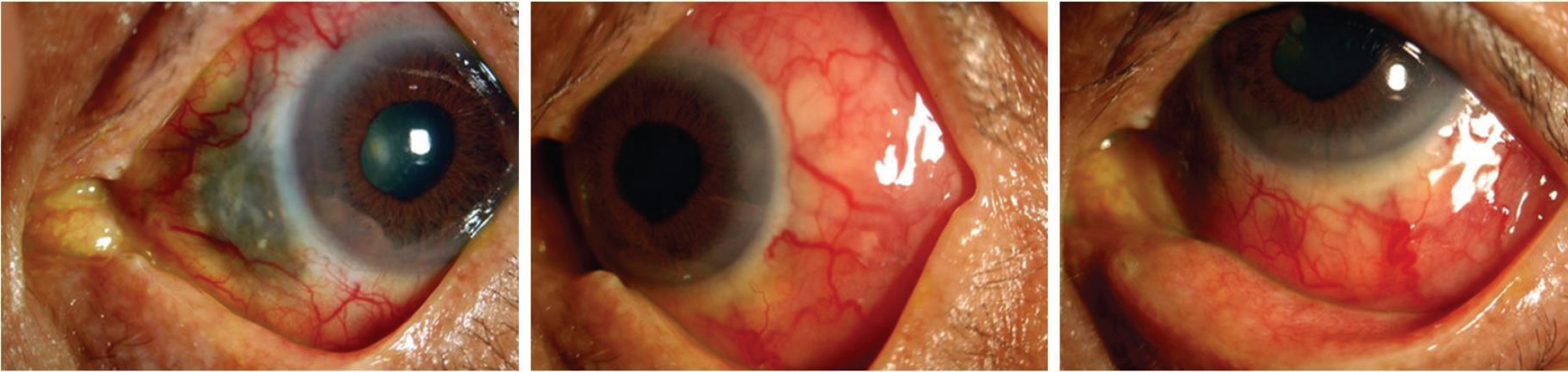
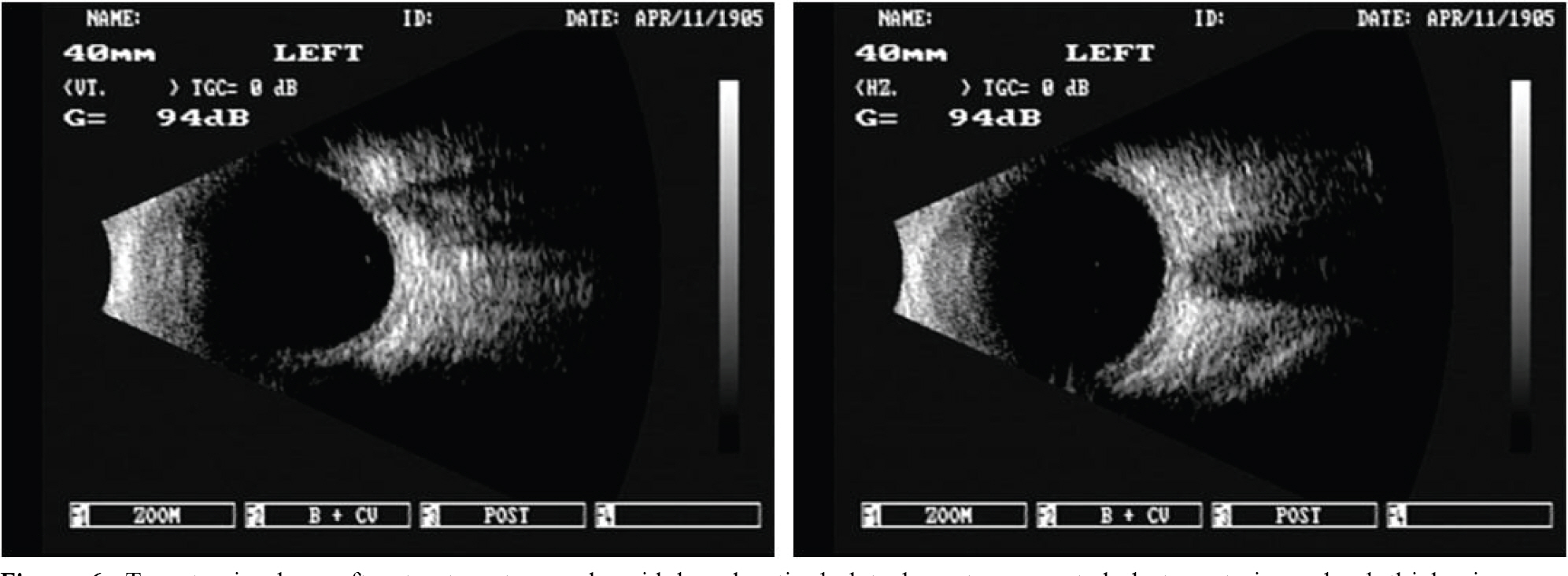
A 71-year-old man presented with orbital cellulitis and diffuse anterior scleritis of his left eye. Although orbital cellulites showed remission with topical and systemic antibiotics, scleritis persisted despite a combination therapy of immunosuppressive agents (cyclosporin, mycophenolate, prednisolone) for 1 month. Finally, he was given infliximab (5 mg/kg) intravenously three times at 2-week intervals, after which ocular pain, chemosis, conjunctival injection, and sclera thickening considerably reduced, and scleritis completely remitted.
CONCLUSIONS
The administration of Infliximab seems to be an effective therapy in patients with intractable scleritis undergoing conventional therapy.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Fong LP, Sainz de la Maza M. . Immunopathology of scleritis. Ophthalmology. 1991; 98:472–9.
Article2. Murphy CC, Ayliffe WH, Booth A. . Tumor necrosis factor alpha blockade with infliximab for refractory uveitis and scleritis. Ophthalmology. 2004; 111:352–6.3. Jabs DA, Mudun A, Dunn JP, Marsh MJ. Episcleritis and scleritis: clinical features and treatment results. Am J Ophthalmol. 2000; 130:469–76.
Article4. Jeoung JW, Yoon YM, Kim MK. The Effect of Amniotic Membrane Transplantation on the Treatment of Necrotizing Scleritis after Pterygium Excision. J Korean Ophthalmol Soc. 2004; 5:1981–4.5. Koizumi K, Poulaki V, Doehman S. . Contribution of TNF-α to leukocyte adhesion, vascular leakage, and apoptotic cell death in endotoxin-induced uveitis in vivo. Invest Ophthalmol Vis Sci. 2003; 44:2184–91.
Article6. Bazzoni F, Beutler B. The tumor necrosis factor ligand and receptor families. N Engl J Med. 1996; 334:1717–24.
Article7. Feldmann M, Maini RN. Anti-TNF-a therapy of rheumatoid arthritis: what have we learned? Annu Rev Immunol. 2001; 19:163–96.8. Sfikakis PP, Kollias G. TNF biology in experimental and clinical arthritis. Curr Opin Rheumatol. 2003; 15:380–6.9. Shin JC, Im CY, Lee JH, Seo KY. Increased Tear TNF-alpha and MMP-9 in Patients with Necrotizing Scleritis after Pterygium Excision. J Korean Ophthalmol Soc. 2004; 5:720–4.10. Sartani G, Silver PB, Rizzo L. . Anti-tumor necrosis factor alpha therapy suppresses the induction of experimental autoimmune uveoretinitis in mice by inhibiting antigen priming. Invest Ophthalmol Vis Sci. 1996; 37:2211–8.11. Mo JS, Matsukawa A, Ohkawara S, Yoshinaga M.Involvement of TNF-α, IL-1β, and IL-1 receptor antagonist in LPS-induced rabbit uveitis. Exp Eye Res. 1998; 66:547–57.12. Forrester JV. Uveitis: pathogenesis. Lancet. 1991; 338:1498–501.
Article13. Reiff A, Takei S, Sadeghi S. . Etanercept therapy in children with treatment-resistant uveitis. Arthritis Rheum. 2001; 44:1411–5.
Article14. Smith JR, Levinson RD, Holland GN. . Differential efficacy of tumor necrosis factor inhibition in the management of inflammatory eye disease and associated rheumatic disease. Arthritis Care Res. 2001; 45:252–7.
Article15. Sobrin L, Kim EC, Christen W. . Infliximab therapy for the treatment of refractory ocular inflammatory disease. Arch Ophthalmol. 2007; 125:895–900.
Article16. Galor A, Perez VL, Hammel JP, Lowder CY. Differential effectiveness of etanercept and infliximab in the treatment of ocular inflammation. Ophthalmology. 2006; 113:2317–23.
Article17. Murphy CC, Ayliffe WH, Booth A. . Tumor necrosis factor alpha blockade with infliximab for refractory uveitis and scleritis. Ophthalmology. 2004; 111:352–6.18. Suhler EB, Smith JR, Wertheim MS. . A prospective trial of infliximab therapy for refractory uveitis. Arch Ophthalmol. 2005; 123:903–12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of a Patient with Refractory Scleritis Treated with Rituximab
- Intravitreal Bevacizumab (Avastin) as an Adjuvant for the Treatment of Posterior Scleritis
- A Case of Nodular Scleritis in Association With Behcet's Disease
- The Efficacy of Infliximab in Refractory Uveitis
- A Case of Post. Scleritis Associated with Ciliochoroidal Detachment and Ant. Uveitis in Background Diabetic Retinopathy Patient