J Korean Ophthalmol Soc.
2007 Dec;48(12):1723-1727.
Lens Particle Glaucoma with Intraocular Foreign Body
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Inje University, Seoul Paik Hospital, Seoul, Korea.
- 2Department of Ophthalmology, Gachon University of Medicine and Science, Gil Medical Center, Incheon, Korea. leedy91@yahoo.co.kr
Abstract
-
PURPOSE: To report a case of acute lens particle glaucoma with an intraocular foreign body that persisted for a long duration.
CASE SUMMARY
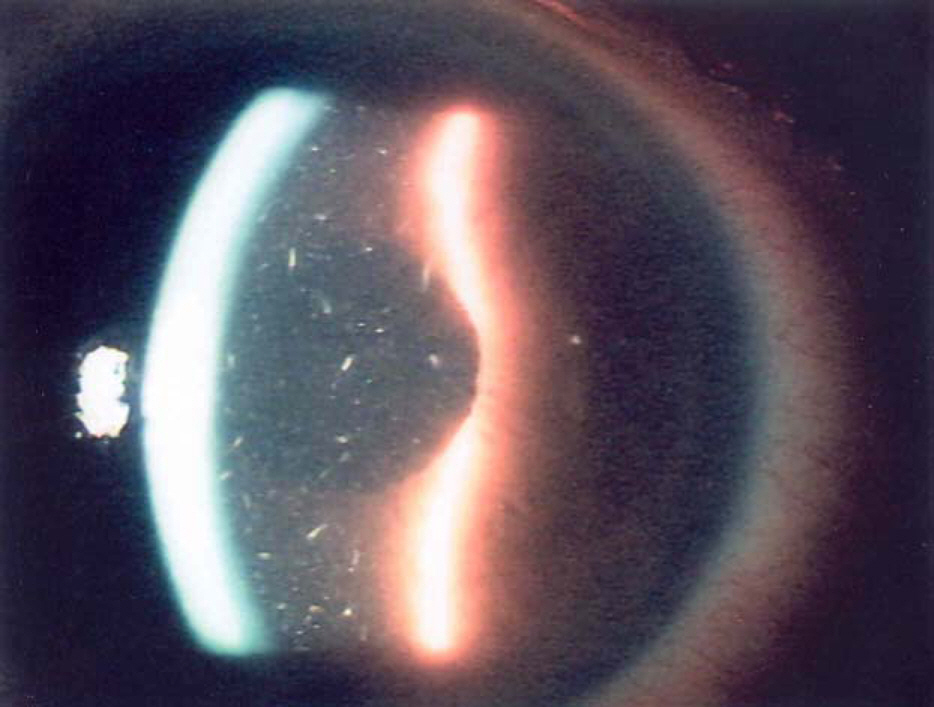
A 47-year-old man visited our clinic due to severe pain in his right eye. His uncorrected visual acuity was hand movement, and intraocular pressure (IOP) measured by a Goldmann applanation tonometer was 76 mmHg in the right eye. Severe corneal edema and floating lens materials in the anterior chamber were revealed by slit-lamp examination. An ultrasonography scan showed that the lens had dislocated into the vitreous cavity and revealed vitreous opacities. To remove lens materials and control IOP, anterior chamber irrigation and trans pars plana vitrectomy with lensectomy were performed under local anesthesia. During the operation, an intraocular foreign body was removed from the anterior chamber. Dislocated lens particles were removed by vitrectomy. After the operation, his best corrected visual acuity was 1.0, and intraocular pressure was 12 mmHg in the right eye.
CONCLUSIONS
Close observation is needed in cases with lens particle glaucoma, because a long-persisting intraocular foreign body can be accompanied by lens particle glaucoma.
MeSH Terms
Figure
Reference
-
References
1. Williams DF, Mieler WF, Abrams GW, Lewis H. Results and prognostic factors in penetrating ocular injuries with retained intraocular foreign bodies. Ophthalmology. 1988; 95:911–6.
Article2. Begle HL. Perforating injuries of the eye by small steel fragments. Am J Ophthalmol. 1929; 12:970–7.
Article3. Barendtrup P. Two cases of temporary siderosis bulbi with spontaneous resoprtion and without impairment of function. Acta Ophthalmol. 1944; 22:311–6.4. Ahn M. Noninfectious endophthalmitis caused by an intraocular foreign body retained for 16 years. J Korean Ophthalmol Soc. 2001; 42:793–6.5. Lin HC, Wang HZ, Lai YH. Occult plastic intravitreal foreign body retained for 30 years: a case report. Kaohsiung J Med Sci. 2006; 22:529–33.
Article6. Allingham RR. Shields’ textbook of glaucoma. 5th ed.Philadelphia: Lippincott Williams & Wilkins;2005. p. 322–5.7. Epstein DL. Diagnosis and management of lens-induced glaucoma. Ophthalmology. 1982; 89:227–30.
Article8. Epstein DL, Jedziniak JA, Grant WM. Obstruction of aqueous outflow by lens particles and by heavy-molecular-weight soluble lens proteins. Invest Ophthlamol Vis Sci. 1978; 17:272–7.9. Kim JH. Cataract. 1st ed.Seoul: Ilchokak;2002. p. 358–9.10. Pieramici DJ, Capone A Jr, Rubsamen PE, Roseman RL. Lens preservation after intraocular foreign body injuries. Ophthalmology. 1996; 103:1563–7.
Article11. Perlman EM, Albert DM. Clinically unsuspected phacoanaphylaxis after ocular trauma. Arch Ophthalmol. 1977; 95:244–6.
Article12. Rahi AHS, Misra RN, Morgan G. Immunology of the lens. Humoral and cellular immune responses to autologous lens antigens and their roles in ocular inflammation. Br J Ophthalmol. 1977; 61:371–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Chamber Intraocular Lens Implantation Combined with Pars Plana Lensectomy and Intraocular Foreign Body Removal
- A Simple Method of X-ray Examination in Detection of Intraocular Foreign Body with Contact Lens Suction Cup
- Removed Intraocular Lenses: A Clinical and Histopathological Study
- Lens particle glaucoma occurring 15 years after cataract surgery
- Posterior Chamber Intraocular Lens Implantation in front of the Anterior Lens Capsule during Pars Plana Lensectomy and Vitrectomy