J Korean Ophthalmol Soc.
2007 Sep;48(9):1202-1211.
Risk Factors Affecting Efficacy of Intracameral Amphotericin Injection in Deep Keratomycosis
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. kmk9@snu.ac.kr
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- 3Department of ophthalmology, Seoul National University Bundang Hospita, Seoul, Korea.
Abstract
-
PURPOSE: To investigate the clinical efficacy of intracameral amphotericin injection and to evaluate risk factors affecting primary treatment success in fungal infection invading the anterior segment of the eye.
METHODS
Twenty-six eyes of 26 patients diagnosed with fungal infection in the anterior segment were studied. The initial treatment regimen was a topical 0.15% amphotericin application and itraconazole oral administration after culture. Amphotericin (5 ug/0.1 ml, 0.1 cc) was repeatedly injected intracamerally when the infection intensified. Penetrating keratoplasty was conducted for eyes unresponsive to intracameral amphotericin injection. The relative risk ratios of ulcer size, infiltration depth, culture positivity, and hypopyon were compared in each treatment group to evaluate the treatment response.
RESULTS
Of patients with fungal infection, 30.7% were cured with intracameral amphotericin injection, while 30.7% needed penetrating keratoplasty. Intracameral amphotericin injection was needed in the presence of large corneal ulcers (>14 mm2), hypopyon, positive fungal culture, use of steroid eye drops, and deep infiltration at initial examination. Large ulcer size (>14 mm2) was the main risk factor for needing penetrating keratoplasty. Of the eyes Candida infection, 66.5% needed evisceration.
CONCLUSIONS
Large ulcer size and the isolation of Candida were poor prognostic factors related to the efficacy of intracameral amphotericin injection.
Keyword
MeSH Terms
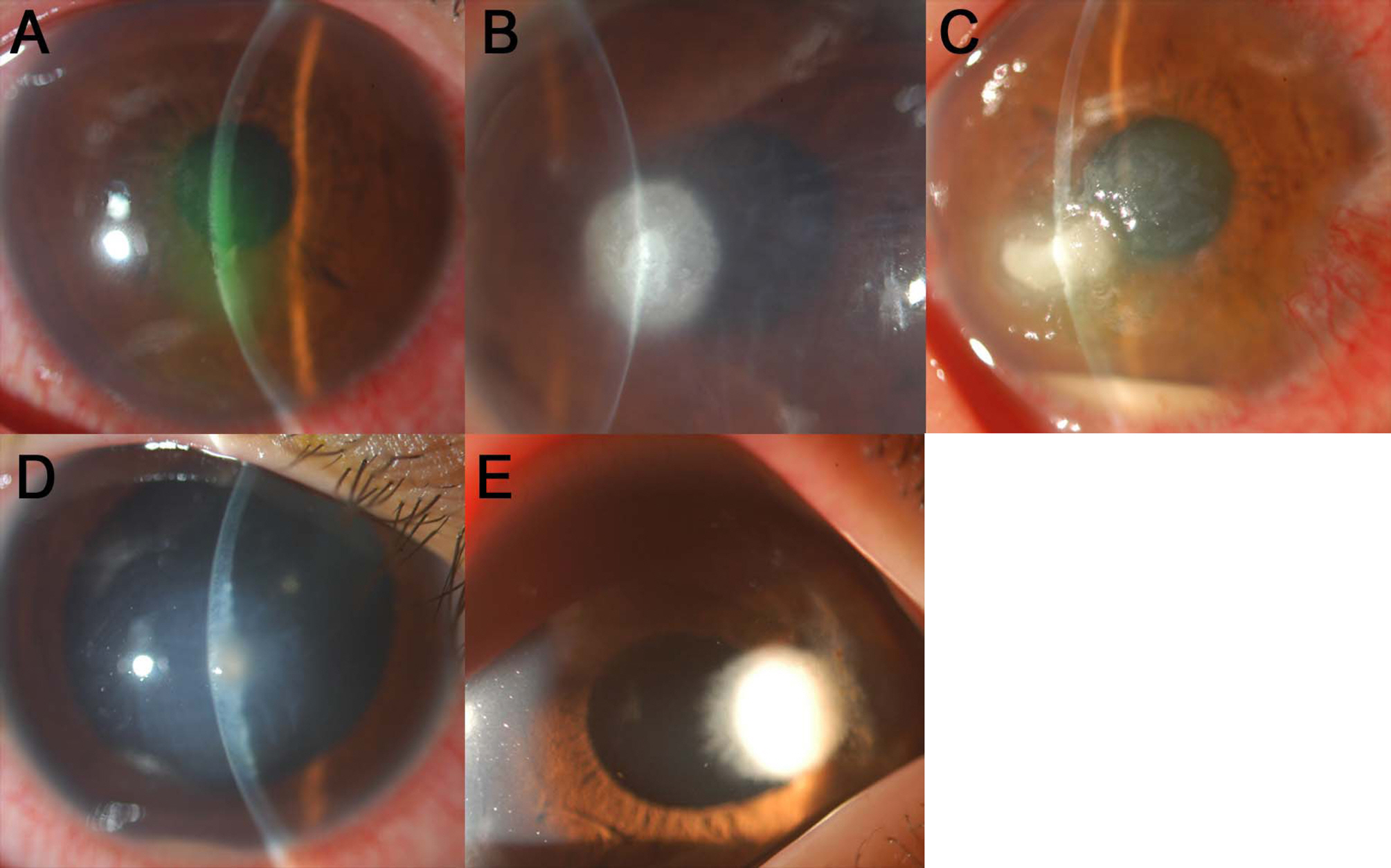
Figure
Reference
-
References
1. Tanure MA, Cohen EJ, Sudensh D, et al. Spectrum of fungal keratitis at Wills Eye Hospital, Philadelphia, Pennsylvania. Cornea. 2000; 19:307–12.
Article2. Chang CW, Ho CK, Chen ZC, et al. Fungi genus and concentration in the air of onion fields and their oppotunistic action related to mycotic keratitis. Arch Environ Health. 2002; 57:349–54.3. Panda A, Sharma N, Das G, et al. Mycotic keratitis in children: epidemiologic and microbiologic evaluation. Cornea. 1997; 16:295–9.4. Bharathi MJ, Ramakrishnan R, Vasu S, et al. Epideiological characteristics and laboratory diagnosis of fungal keratitis: a three-year study. Indian J Ophthalmol. 2003; 51:315–21.5. Srinivasan M, Gonzales CA, George C, et al. Epidemiology and aetiological diagnosis of corneal ulceration in Madurai, south India. Br J Ophthalmol. 1997; 81:965–71.
Article6. Srinivasan M. Fungal keratitis. Curr Opin Ophthalmol. 2004; 15:321–7.
Article7. O'Day DM. Selection of appropriate antifungal therapy. Cornea. 1987; 6:238–45.8. O'Day DM, Head WS, Robinson RD, Clanton JA. Corneal penetration of topical amphotericin B and natamycin. Curr Eye Res. 1986; 5:877–82.9. Kaushik S, Ram J, Brar GS, et al. Intracameral amphotericin B Initial experience in severe keratomycosis. Cornea. 2001; 20:715–9.10. Xie L, Dong X, Shi W. Treatment of fungal keratitis by penetrating keratoplasty. Br J Ophthalmol. 2001; 85:1070–4.
Article11. Panda A, Vajpayee RB, Kumar TS. Critical evaluation of therapeutic keratoplasty in cases of keratomycosis. Ann Ophthalmol. 1991; 23:373–6.12. Myung NH, Yang YS, Kim JD. The result of surgical managements of three case of refractory fungal corneal ulcer. J Korean Ophthalmol Soc. 1994; 35:1572–6.13. Lalitha P, Prajna NV, Kabra A, et al. Risk factors for treatment outcome in fungal keratitis. Ophthalmology. 2006; 113:526–30.
Article14. Jones DB. Initial therapy of suspected microbial corneal ulcers: Specific antibiotics therapy based on corneal smears. Surv Ophthalmol. 1979; 24:105–16.15. Mah-Sadorra JH, Najjar DM, Rapuano CJ, et al. Serrtia corneal ulcers :a retrospective clinical study. Cornea. 2005; 24:793–800.16. Morlet N, Minassian D, Butcher J. Risk factors for treatment outcome of suspected microbial keratitis. Ofloxacin Study Group. Br J Ophthalmol. 1999; 83:1027–31.17. Wilhelm us KR, Schlech BA. Clinical and epidemiological advantages of culturing bacterial keratitis. Cornea. 2004; 23:38–42.
Article18. Souri EN, Green WR. Intravitreal amphotericin-B toxicity. Am J Ophthalmol. 1974; 78:77–81.19. Kuriakose T, Kothari M, Paul P, et al. Intracameral amphotericin B injection in the management of deep keratomycosis. Cornea. 2002; 21:653–6.
Article20. Park SH, Kim MS. A case report of intracameral amphotericin B injection in the management of deep keratomycosis. J Korean Ophthalmol Soc. 2004; 45:681–5.21. Gopinathan U, Garg P, Fernandes M, et al. The epidemiological features and laboratory results of fungal keratitis: a 10-year review at a referral eye care center in South India. Cornea. 2002; 21:555–9.22. Jones BR. Principles in the management of oculomycosis. Am J Ophthalmol. 1975; 79:719–51.
Article23. Gotz VP, Mar DD, Roche JJ. Compatibility of amphotericin B with drugs used to reduce adverse reations. Am J Hosp Pharm. 1981; 38:378–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of Intracameral Amphotericin B Injection in the Management of Deep Keratomycosis
- Clinical Effects of Intracameral Voriconazole Injection in Patients with Fungal Keratitis Refractory to Conventional Treatment
- A Case of Iris Neovascularization in Severe Fungal Keratitis Treated with Intracameral Bevacizumab
- Retinal Toxicity of Repetitive Intravitreal Injections of Amphotericin B
- Efficacy and Safety of Intracameral Bevacizumab for Treatment of Neovascular Glaucoma