J Korean Ophthalmol Soc.
2007 Sep;48(9):1189-1195.
Comparison of Graft Rejection of First Eyes and Second Eyes after Bilateral Penetrating Keratoplasty
- Affiliations
-
- 1Department of Ophthalmology, Gangnam St, Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. mskim@catholic.ac.kr
- 2Department of Ophthalmology, Uijongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Gyeonggi, Korea.
Abstract
-
PURPOSE: To compare graft rejection of the first and second eyes after bilateral penetrating keratoplasty.
METHODS
We performed a retrospective review of the cases of 16 patients who underwent bilateral penetrating keratoplasty. Nonparametric Kaplan-Meier survival analysis was used to account for variable follow-up among patients.
RESULTS
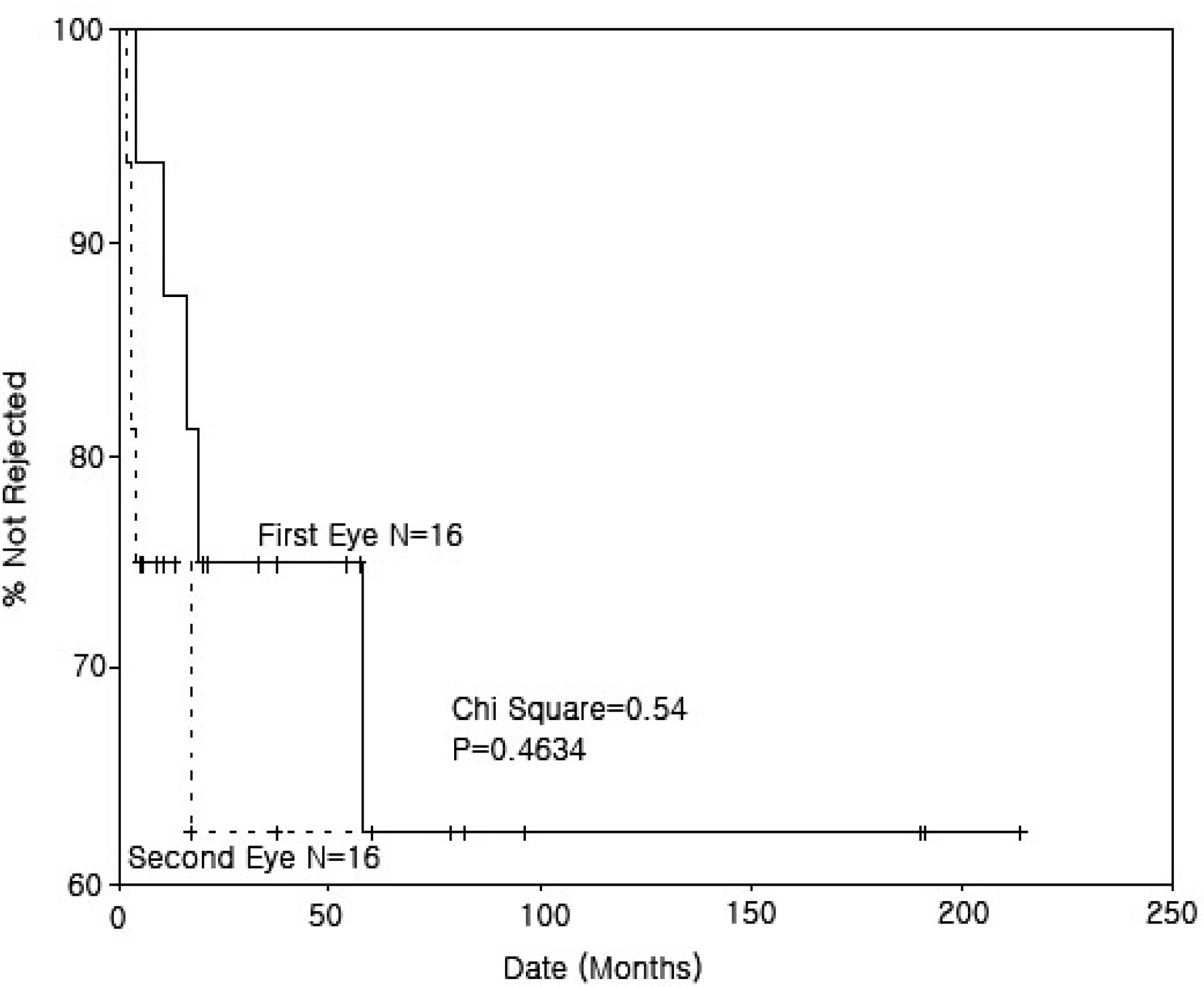
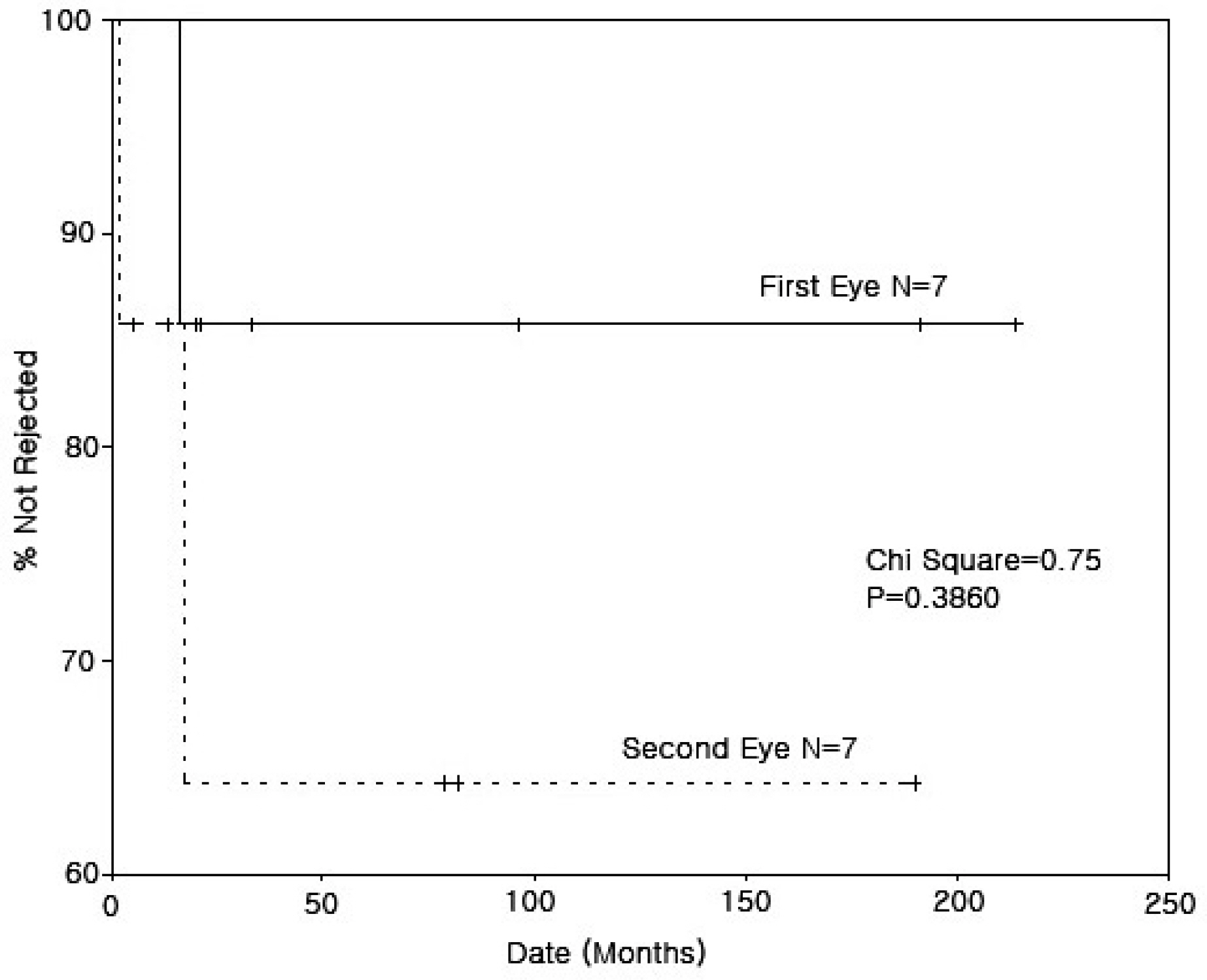
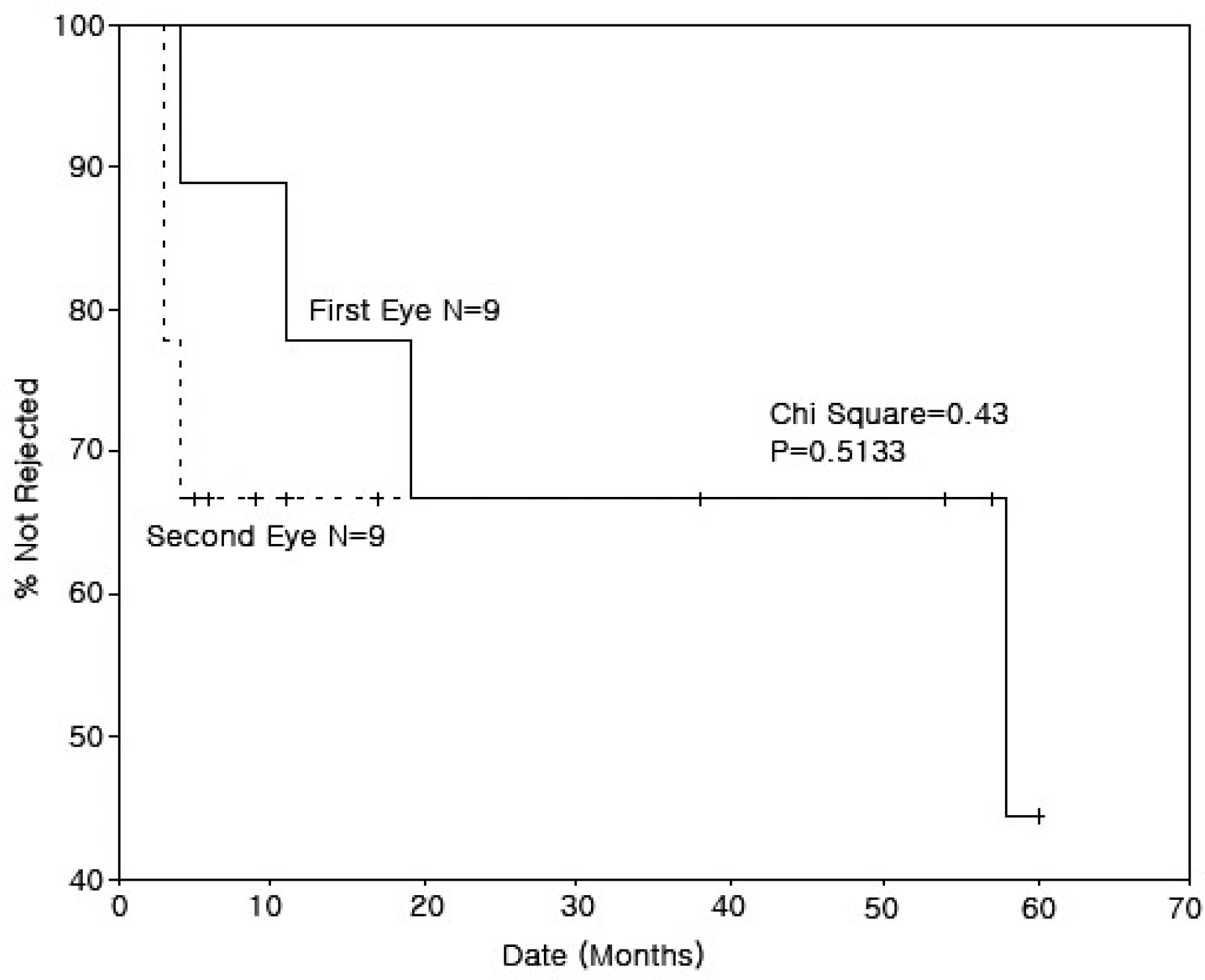
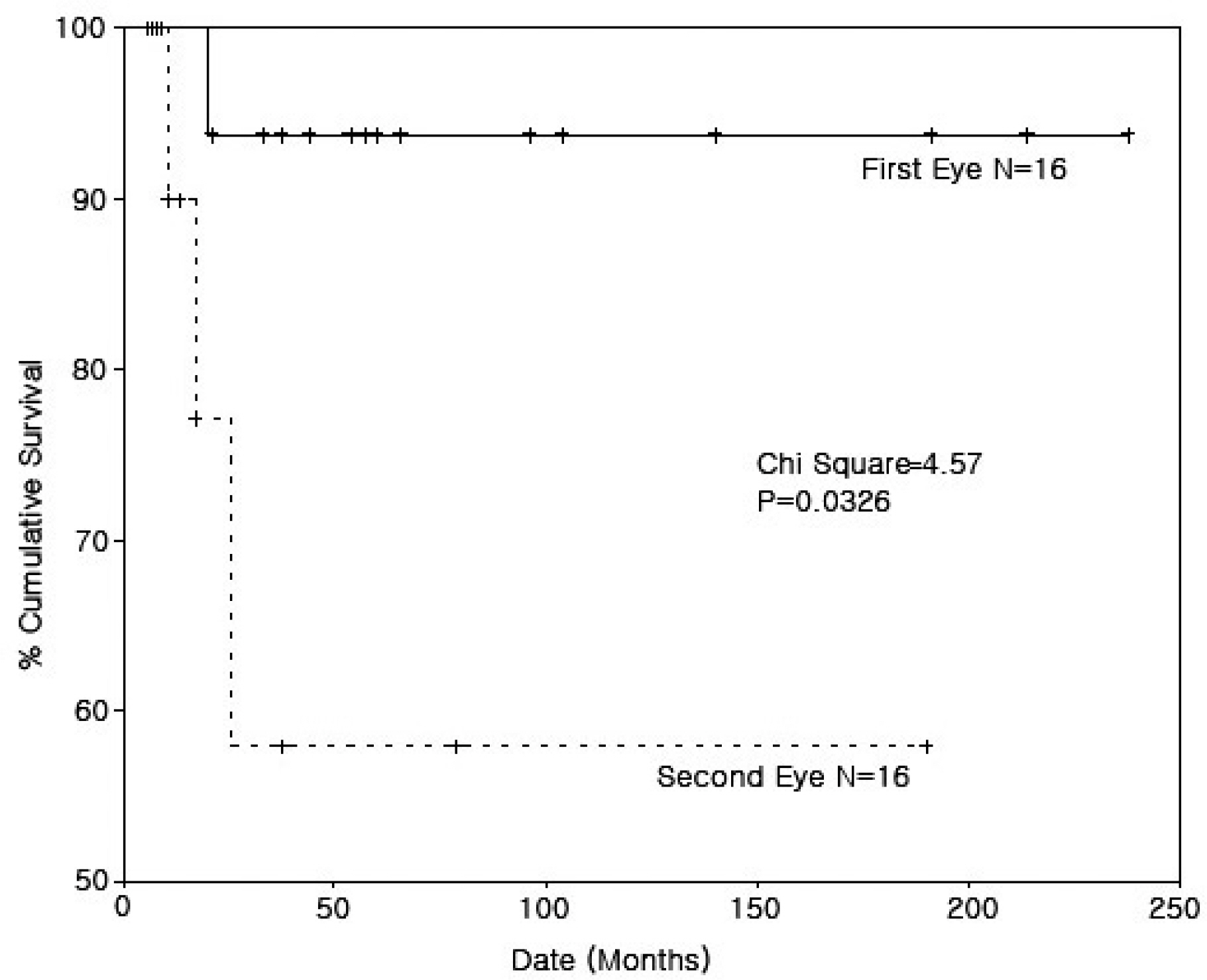
The mean age of the 16 patients (12 M, 4 F) was 39.1 years. Mean follow-up was 89.8 months after surgery in the first eye and 42.8 months after surgery in the second eye. The average time interval between surgery on the first and second eyes was 47.0 months. The indications for surgery were keratoconus (37.5%), corneal dystrophy (25.0%), pseudophakic bullous keratopathy (12.5%), band keratopathy (12.5%), and inflammatory corneal opacity (12.5%). Endothelial rejection occurred in five of the first eyes but was treated successfully, remaining clear until the last follow-up. Endothelial rejections were seen in five of the second eyes, two of which failed. Survival analysis of endothelial rejection showed no significant difference between the first and second eyes; however, survival analysis of the graft failure showed a decreased survival rate of the second eyes compared with that of the first eyes. The best corrected visual acuity at the last follow-up of the second eyes seemed to be worse than that of the first eyes.
CONCLUSIONS
Survival analysis of the endothelial rejections showed no significant difference between the first and second eyes. Survival analysis of the graft failure showed decreased survival rate of the second eyes. At the last follow-up the best corrected visual acuity of the second eyes appeared to be worse than that of the first eyes.
MeSH Terms
Figure
Reference
-
References
1. Tuft SJ, Greory WM, Davison CR. Bilateral Penetrating Keratoplasty for Keratoconus. Ophthalmology. 1995; 102:462–8.
Article2. Choi SH, Lee YW, Kim HM, et al. Epidemiologic Studies of Keratoplasty in Korea. J Korean Ophthalmol Soc. 2006; 47:538–47.3. Musch DC, Myer RF. Risk of Endothelial Rejection after Bilateral Penetrating Keratoplasty. Ophthalmology. 1989; 96:1139–43.
Article4. Khodadoust AA, Karnema Y. Corneal Grafts in the Second Eye. Cornea. 1984; 3:17–20.
Article5. Park SH, Kim JH, Joo CK. The Clinical Evaluations of the Penetrating Keratoplasty with Imported Donor Corneas. J Korean Ophthalmol Soc. 2005; 46:28–34.6. Kim EC, Kim MS. Graft Rejection in Penetrating Keratoplasty. J Korean Ophthalmol Soc. 2003; 44:289–95.7. Rao SK, Sudhir RR, Fogla R, et al. Bilateral Penetrating Keratoplasty- Indications, Results and Review of Literature. Int Ophthalmol. 2001; 23:161–6.8. Arentsen JJ. Corneal Transplant Allograft Reaction: Possible Predisposing Factors. Trans Am Ophthalmol Soc. 1983; 81:361–402.9. Chandler JM, Kaufman HE. Graft Reactions after Keratoplasty for Keratoconus. Am J Ophthalmol. 1974; 77:543–7.
Article10. Pouliquen Y, Rocher C. Keratoplasties successives et maladie du greffon. Arch Ophthalmol. 1975; 35:847–64.11. Malbran ES, Fernandez-Meijide RE. Bilateral versus Unilateral Penetrating Graft in Keratoconus. Ophthalmology. 1982; 89:38–40.
Article12. Buxton JN, Schuman M, Pecego J. Graft Reactions after Unilateral and Bilateral Keratoplasty for Keratoconus. Ophthalmology. 1981; 88:771–3.
Article13. Ruedemann AD Jr.Clinical Course of Keratoconus. Trans Am Acad Ophthal Otolaryng. 1970; 74:384–98.14. Donshik PC, Cavanagh HD, Boruchoff SA, Dohlman CH. Effect of Bilateral and Unilateral Grafts on the Incidence of Rejections in Keratoconus. Am J Ophthalmol. 1979; 87:823–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Results of Graft Rejection after Unilateral and Bilateral Keratoplasty in Keratoconus
- Clinical Results of Graft Rejection Related to Graft Size after Keratoplasty in Keratoconus
- Clinical Evaluation of the Graft Rejection after Penetrating Keratoplasty
- A Clinical Study of Risk Factors of Graft Rejection for Penetrating Keratoplasty
- Clinical Analysis of Penetrating Keratoplasty in Herpes Simplex Keratitis