J Korean Surg Soc.
2012 May;82(5):312-316.
Measuring the stress of the surgeons in training and use of a novel interventional program to combat it
- Affiliations
-
- 1Division of Investigative Science, Department of Medicine, Imperial College London Faculty of Medicine, London, UK. i.christakis@imperial.ac.uk
- 2Postgraduate Course Stress Management and Health Promotion, University of Athens School of Medicine, Athens, Greece.
- 3First Department of Paediatrics, Children's Hospital Aghia Sofia, University of Athens School of Medicine, Athens, Greece.
Abstract
- PURPOSE
Stress poses a serious risk for training surgeons since their performance and well-being in reflected in patients' health. This study focuses on measuring the stress of training surgeons and at the same time evaluates prospectively the results of an innovative program that uses alternative techniques to combat the effects of stress.
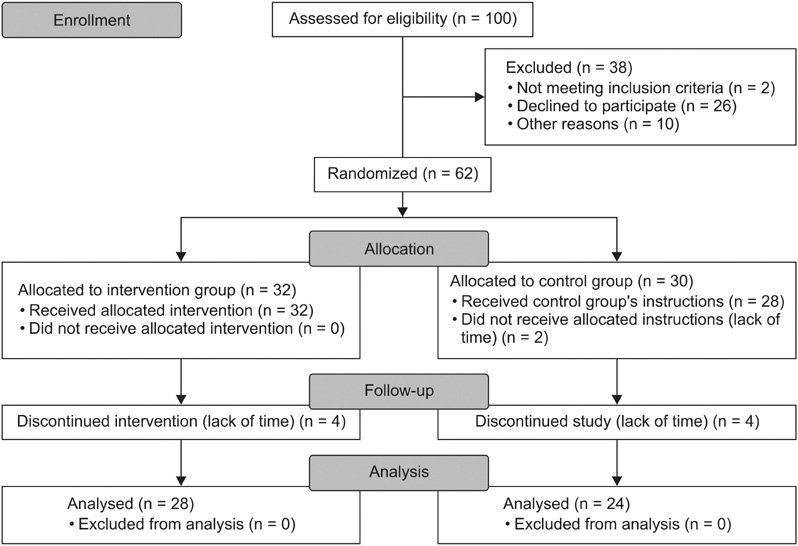
METHODS
The study was a pilot randomized controlled trial, with a duration of 6 months. Participants were allocated to a control and an intervention group. Trainees then completed three questionnaires, quality of life, perceived stress scale (PSS) and job content questionnaire serving as a baseline measurement. Only the intervention group used diaphragmatic breathing and progressive muscular relaxation techniques, twice a day, for 20 minutes each, and for a total period of eight weeks. At the end of the study, the same questionnaires were completed again by both groups.
RESULTS
The sample of the study included 28 and 32 trainees in the control and the intervention group, respectively. The Cronbach's alpha value for the PSS stress-measuring questionnaire was 0.772. The intervention group presented statistically significant lower values of stress (30.50, P < 0.05) in comparison to the control group (27.54).
CONCLUSION
The medical community, and especially surgeons, have been reluctant up to now to embrace interventional programs that go beyond the traditional use of medication in order to address stress related issues. The positive results and feedback from small studies, such as ours, can provide the driving force for further research that will give us solid, evidence-based, answers.
MeSH Terms
Figure
Reference
-
1. Buddeberg-Fischer B, Klaghofer R, Stamm M, Siegrist J, Buddeberg C. Work stress and reduced health in young physicians: prospective evidence from Swiss residents. Int Arch Occup Environ Health. 2008. 82:31–38.2. Schmidt TS, Dembroski TM, Bluümchen G. Biological and psychological factors in cardiovascular disease. 1986. Berlin: Springer.3. Theorell T. Berkman LF, Kawachi I, editors. Social epidemiology. Social epidemiology. 2000. New York: Oxford University Press;95–117.4. Harms BA, Heise CP, Gould JC, Starling JR. A 25-year single institution analysis of health, practice, and fate of general surgeons. Ann Surg. 2005. 242:520–526.5. Campbell DA Jr, Sonnad SS, Eckhauser FE, Campbell KK, Greenfield LJ. Burnout among American surgeons. Surgery. 2001. 130:696–702.6. Bartle EJ, Sun JH, Thompson L, Light AI, McCool C, Heaton S. The effects of acute sleep deprivation during residency training. Surgery. 1988. 104:311–316.7. Browne BJ, Van Susteren T, Onsager DR, Simpson D, Salaymeh B, Condon RE. Influence of sleep deprivation on learning among surgical house staff and medical students. Surgery. 1994. 115:604–610.8. Deaconson TF, O'Hair DP, Levy MF, Lee MB, Schueneman AL, Codon RE. Sleep deprivation and resident performance. JAMA. 1988. 260:1721–1727.9. Godellas CV, Huang R. Factors affecting performance on the American Board of Surgery in-training examination. Am J Surg. 2001. 181:294–296.10. Goldman LI, McDonough MT, Rosemond GP. Stresses affecting surgical performance and learning. I. Correlation of heart rate, electrocardiogram, and operation simultaneously recorded on videotapes. J Surg Res. 1972. 12:83–86.11. Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J. Laparoscopic performance after one night on call in a surgical department: prospective study. BMJ. 2001. 323:1222–1223.12. Haynes DF, Schwedler M, Dyslin DC, Rice JC, Kerstein MD. Are postoperative complications related to resident sleep deprivation? South Med J. 1995. 88:283–289.13. Light AI, Sun JH, McCool C, Thompson L, Heaton S, Bartle EJ. The effects of acute sleep deprivation on level of resident training. Curr Surg. 1989. 46:29–30.14. Taffinder NJ, McManus IC, Gul Y, Russell RC, Darzi A. Effect of sleep deprivation on surgeons' dexterity on laparoscopy simulator. Lancet. 1998. 352:1191.15. Wetzel CM, Kneebone RL, Woloshynowych M, Nestel D, Moorthy K, Kidd J, et al. The effects of stress on surgical performance. Am J Surg. 2006. 191:5–10.16. Rowe MM. Teaching health-care providers coping: results of a two-year study. J Behav Med. 1999. 22:511–527.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Endoscopy Training in Korea and Future Aspects
- Perspectives on Fellowship Training Standard in Interventional Neuroradiology
- International Survey on Criteria for Training and Accreditation in Interventional Neuroradiology
- Development and Effects of a Resilience Training Program for Nurses
- Residency training: training program renewal and evaluation of training