J Korean Soc Transplant.
2011 Jun;25(2):87-94.
Liver Regeneration and Factors Influencing Liver Regeneration in Donors and Recipients of Adult Living Donor Liver Transplantation Using Right Lobe Graft
- Affiliations
-
- 1Department of Surgery, Seoul St. Mary's Hospital, The Catholic University of Korea, College of Medicine, Seoul, Korea. kimdg@catholic.ac.kr
Abstract
- BACKGROUND
To balance between the appropriate remnant liver volume in the donors and sufficient graft volume in the recipients is very important in adult living donor liver transplantation (LDLT). The aim of this study is to evaluate the liver regeneration rate and the factors associated with the regenerative process in the donors and recipients.
METHODS
Between May 1999 and March 2010, 197 donors and 98 recipients out of the 450 patients who underwent adult LDLT were evaluated retrospectively. We reviewed the clinical characteristics of the patients, liver regeneration using computerized tomography (CT)-assisted volumetry technique and the factors associated with liver regeneration in the donors and recipients.
RESULTS
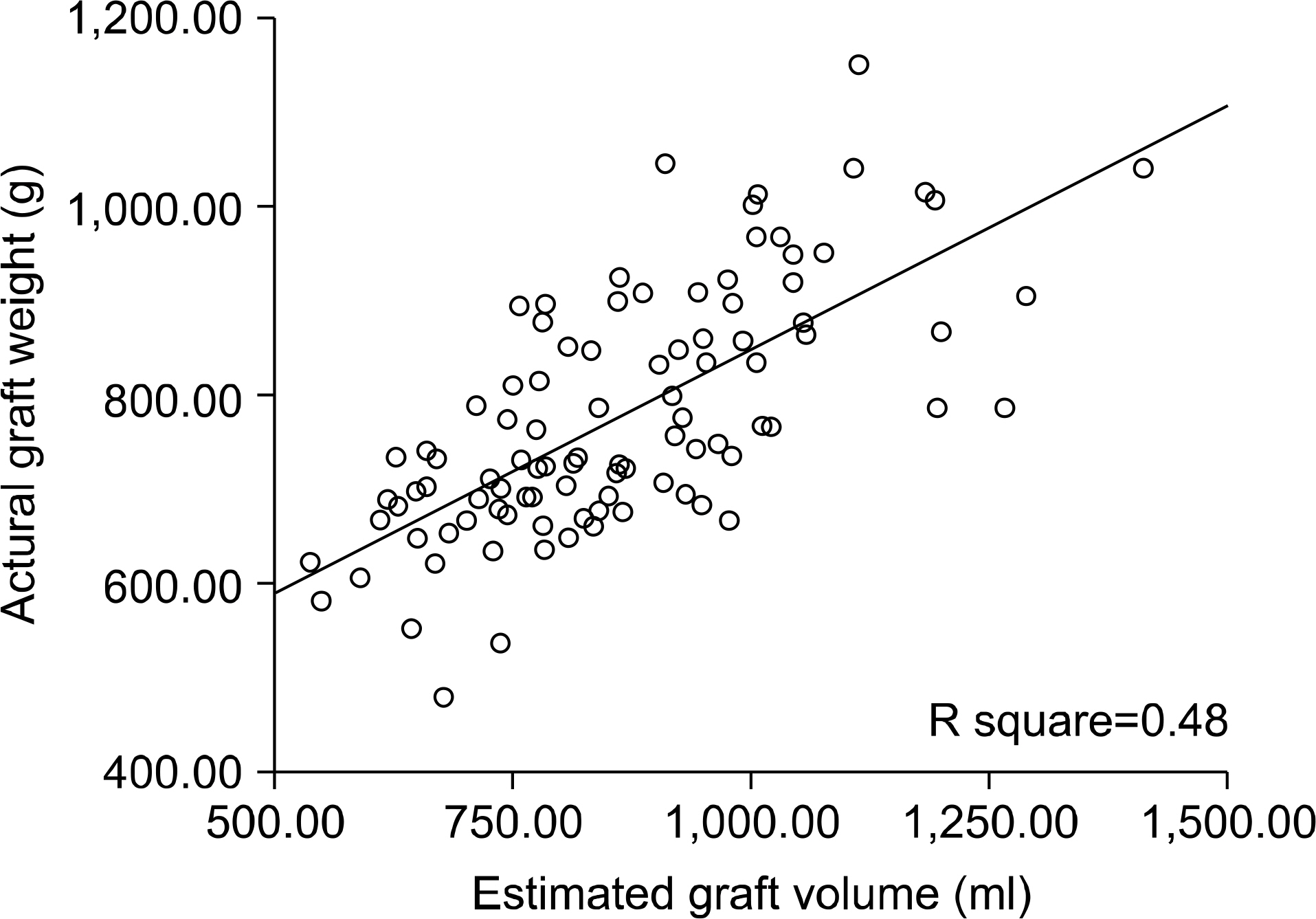
Using CT-assisted volumetry, the mean proportion of remnant right liver lobe was 62.4%+/-4.7%, ranging from 50.1% to 77.4%. The ratio of the graft weight to volume by CT-assisted volumetry was 89.8%+/-12.9% and we created a formula that graft volume (g)=[CT volume (mL)x0.933]+137.97. The liver regeneration rate in donors during the first postoperative week was higher if the remnant liver volume was below 35% than if the remnant liver volume above 35% (p<0.001). After 6 months, the remnant liver grew up to 81.2% of the original liver volume. Liver regeneration in recipients during the first postoperative week was faster if the graft-to-recipient body weight ratio (GRWR) was below 1% than if the GRWR was above 1% (p<0.001). Also, GRWR (p<0.001), portal vein (PV) velocity (cm/sec) (P=0.007) and PV flow volume per 100 g of graft tissue (mL/min) (P=0.002) were associated with liver regeneration in recipients during the early postoperative period by univariate analysis.
CONCLUSIONS
The process of liver regeneration was most active during the first postoperative week in both the donors and recipients. The proportion of remnant liver in donors, GRWR and portal blood flow in recipients appeared to be the significant factors associated with liver regeneration.
MeSH Terms
Figure
Reference
-
References
1). Yamanaka N, Okamoto E, Kawamura E, Kato T, Oriyama T, Fujimoto J, et al. Dynamics of normal and injured human liver regeneration after hepatectomy as assessed on the basis of computed tomography and liver function. Hepatology. 1993; 18:79–85.
Article2). Pachowka M, Zegarska J, Ciecierski R, Korczak-Kowalska G. The role of IL-6 during the late phase of liver regeneration. Ann Trasplant. 2008; 13:15–9.3). Stone HH, Long WD, Smith RB 3rd, Haynes CD. Physiologic consideration in major hepatic resection. Am J Surg. 1969; 117:78–84.4). Haga J, Shimazu M, Wakabayashi G, Tanabe M, Kawachi S, Fuchimoto Y. et al. Liver regeneration in donors and adult recipients after living donor liver transplantation. Liver Transpl. 2008; 14:1718–24.5). Ikegami T, Nishizaki T, Yanaga K, Shimada M, Kishikawa K, Nomoto K, et al. The impact of donor age on living donor liver transplantation. Transplantation. 2000; 70:1703–07.
Article6). Jin MB, Shimamura T, Taniguchi M, Nagasako Y, Suzuki T, Kamiyama T, et al. Liver regeneration in living donor liver transplantation. Nippon Geka Gakkai Zasshi. 2004; 105:674–9.7). Kim SJ, Kim DG, Chung ES, Lee YJ, Moon IS, Lee MD. Adult living donor liver transplantation using the right lobe. Transplant Proc. 2006; 38:2117–20.
Article8). Jiang SM, Zhou GW, Zhang R, Peng CH, Yan JQ, Wan L, et al. Role of splanchnic hemodynamics in liver regeneration after living donor liver transplantation, Liver Transpl. 2009; 15:1043–9.9). Bolognesi M, Sacerdoti D, Bombonato G, Merkel C, Sartori G, Merenda R, et al. Change in portal flow after liver transplantation: effort on hepatic arterial resistance indices and role of spleen size. Hepatology. 2002; 35:601–8.10). Park MY, Lee YJ, Rha SE, Oh SN, Byun JY, Kim DG. Correlation of portal venous velocity and portal venous flow with short term graft regeneration in recipients of living donor liver transplants. Transplant Proc. 2008; 40:1488–91.11). Cheng YF, Huang TL, Chen TY, Tsang LL, Ou HY, Yu CY, et al. Liver graft regeneration in right lobe adult living donor liver transplantation, Am J Transplant. 2009; 9:1382–8.12). Ohira M, Ishifuro M, Ide K, Irei T, Tashiro H, Itamoto T, et al. Significant correlation between spleen volume and thrombocytopenia in liver transplant patients; a concept for predicting persistent thrombocytopenia. Liver Transpl. 2009; 15:208–15.
Article13). Chen HL, Chen CL, Huang TL, Chen TY, Tsang LL, Ou HY, et al. Regeneration rate of left liver grafts in adult living donor liver transplant. Transplant Proc. 2010; 42:699–700.
Article14). Kim J, Yi NJ, Shin WY, Kim T, Lee KU, Suh KS. Platelet transfusion can be related to liver regeneration after living donor liver transplant. World J Surg. 2010; 34:1052–8.15). Fukuhara T, Umeda K, Toshima T, Takeishi K, Morita K, Nagata S, et al. Congestion of the donor remnant right liver after extended left lobe donation. Transpl Int. 2009; 22:837–44.
Article16). Akamatsu N, Sugawara Y, Kaneko J, Sano K, Imamura H, Kokudo N, et al. Effects of middle hepatic vein reconstruction on right liver graft regeneration. Transplantation. 2003; 76:832–7.
Article17). Akamatsu N, Sugawara Y, Tamura S, Kaneko J, Matsui Y, Togashi J, et al. Impact of live donor age (> or=50) on liver transplantation. Transplant Proc. 2007; 39:3189–93.18). Lodewijk L, Mall A, Spearman CW, Kahn D. Effect of liver regeneration on the pharmacokinetics of immunosuppressive drugs. Transplant Proc. 2009; 41:379–81.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Regeneration of graft liver in adult-to-adult living donor liver transplantation using a left lobe graft
- An Analysis on the Usefulness of Concomitant Procurement of the Caudate Lobe in Living Donor Liver Transplantation Using a Left Lobe Graft
- Postoperative Liver Regeneration and Complication In Live Liver Donor after Partial Hepatectomy for Living Donor Liver Transplantation
- Current Status and Perspectives of Living Donor Liver Transplantation
- Donor Safety in Living Donor Liver Transplantation Using Right Lobe