Tuberc Respir Dis.
2010 Nov;69(5):368-374.
Relation between Subjective Symptoms and Rhinolaryngoscopic Findings or Sputum Eosinophilia in Chronic Cough Patients
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 2Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ymoh55@amc.seoul.kr
- 3Department of Allergy, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Asthma Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
Abstract
- BACKGROUND
Rhinolaryngoscopy and sputum examination are popular tests for the evaluation of chronic cough. Little is known about the relationship between symptoms and rhinolaryngoscopic findings or sputum eosinophilia in chronic cough patients.
METHODS
One hundred patients, who had chronic cough with normal chest radiography and who also had undergone both rhinolaryngoscopy and induced sputum analysis, were reviewed retrospectively. Eleven associated symptoms of chronic cough were asked; postnasal drip (PND) and laryngopharyngeal reflux (LPR) were examined by rhinolaryngoscopy. Induced sputum analysis was performed for evaluation of sputum eosinophilia. Cross tabulation analyses with chi-square tests were used to evaluate the relationship between symptoms and objective findings.
RESULTS
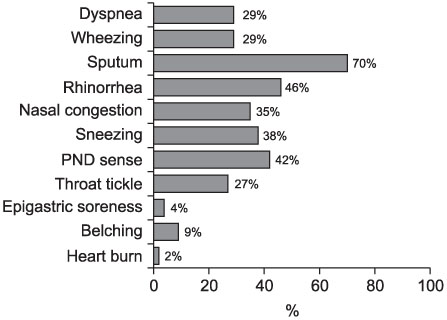
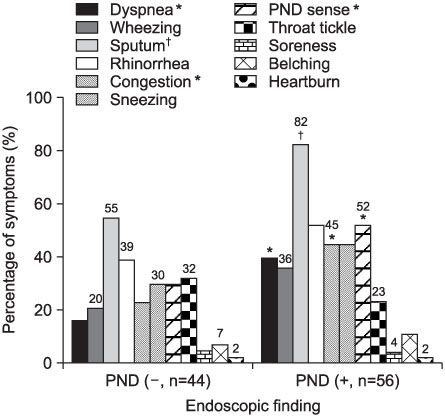
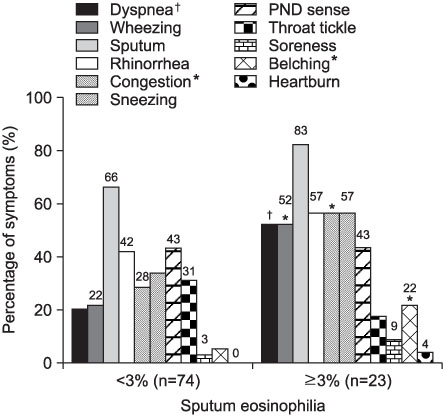
The most frequent symptom was sputum (70%). The prevalence of PND and LPR on rhinolaryngoscopy were 56% (56/100) and 25.6% (22/86), respectively. Sputum eosinophilia was observed in 23 (23.7%) of 97 patients. The dyspnea (p=0.001), sputum (p=0.003), nasal obstruction (p=0.023), and postnasal drip sense (p=0.025) were related with PND on rhinolaryngoscopy. LPR on rhinolaryngoscopy was not related with any symptoms. Dyspnea (p=0.003), wheezing (p=0.005), nasal obstruction (p=0.013), and belching (p=0.018) were related with sputum eosinophilia.
CONCLUSION
Any symptoms might not be related with LPR on laryngoscopy. Some symptoms might be related with PND on rhinoscopy or with sputum eosinophilia.
Keyword
MeSH Terms
Figure
Reference
-
1. Irwin RS, Madison JM. The diagnosis and treatment of cough. N Engl J Med. 2000. 343:1715–1721.2. Pratter MR. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest. 2006. 129:1 Suppl. 63S–71S.3. Koufman JA, Aviv JE, Casiano RR, Shaw GY. Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg. 2002. 127:32–35.4. Belafsky PC, Postma GN, Koufman JA. The validity and reliability of the reflux finding score (RFS). Laryngoscope. 2001. 111:1313–1317.5. Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI). J Voice. 2002. 16:274–277.6. Sohn SW, Yang MS, Lee SH, Song WJ, Lee SM, Kwon HS, et al. Evaluation of the causes of chronic cough with sputum eosinophilia. Korean J Asthma Allergy Clin Immunol. 2007. 27:125–130.7. Kwon NH, Oh MJ, Min TH, Lee BJ, Choi DC. Causes and clinical features of subacute cough. Chest. 2006. 129:1142–1147.8. Mello CJ, Irwin RS, Curley FJ. Predictive values of the character, timing, and complications of chronic cough in diagnosing its cause. Arch Intern Med. 1996. 156:997–1003.9. McGarvey LP, Heaney LG, Lawson JT, Johnston BT, Scally CM, Ennis M, et al. Evaluation and outcome of patients with chronic non-productive cough using a comprehensive diagnostic protocol. Thorax. 1998. 53:738–743.10. Stankiewicz JA, Chow JM. Nasal endoscopy and the definition and diagnosis of chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2002. 126:623–627.11. Ylitalo R, Lindestad PA, Ramel S. Symptoms, laryngeal findings, and 24-hour pH monitoring in patients with suspected gastroesophago-pharyngeal reflux. Laryngoscope. 2001. 111:1735–1741.12. Brightling CE, Ward R, Goh KL, Wardlaw AJ, Pavord ID. Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med. 1999. 160:406–410.13. Wark PA, Gibson PG, Fakes K. Induced sputum eosinophils in the assessment of asthma and chronic cough. Respirology. 2000. 5:51–57.14. Pratter MR, Bartter T, Akers S, DuBois J. An algorithmic approach to chronic cough. Ann Intern Med. 1993. 119:977–983.15. Selner JC. Visualization techniques in the nasal airway: their role in the diagnosis of upper airway disease and measurement of therapeutic response. J Allergy Clin Immunol. 1988. 82:909–916.