Tuberc Respir Dis.
2008 Oct;65(4):339-342.
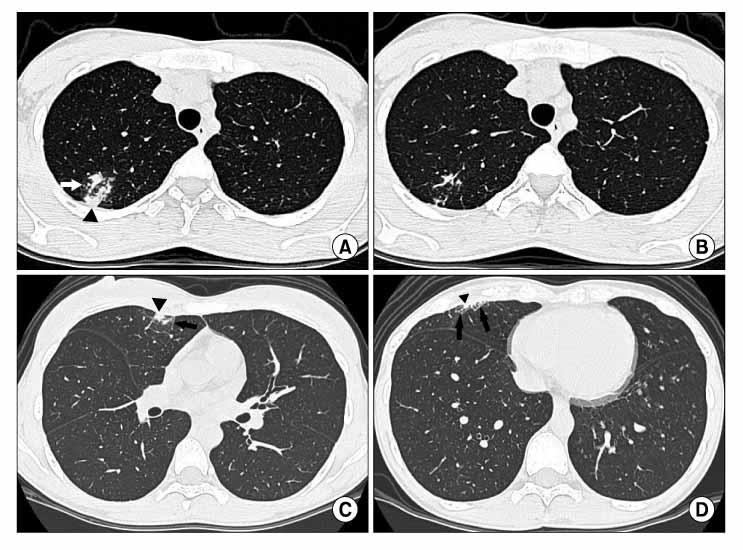
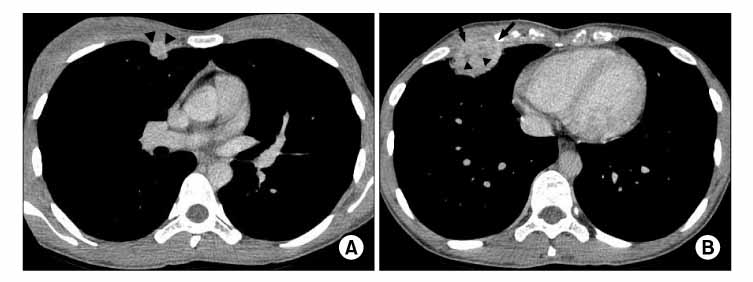
A Case of Transient Radiographic Progression during Treatment of Pulmonary Tuberculosis: Early CT Findings
- Affiliations
-
- 1Department of Diagnostic Radiology, Pochon Cha University College of Medicine, Bundang, Korea.
- 2Department of Diagnostic Radiology, Chung-Ang University College of Medicine, Seoul, Korea. hynlee1@hanmail.net
Abstract
- Early CT findings of transient radiographic progression (TRP) during treatment of active pulmonary tuberculosis including subpleural, interlobular or intralobular septal thickening and micronodules are shown in the present case. Late CT findings of TRP are subpleural, enhancing nodular infiltration with internal low attenuation. These CT features accompanied by a lack of clinical worsening in young patients taking antituberculous medication due to pulmonary tuberculosis can help to differentiate TRP from other disease entities.
Keyword
Figure
Reference
-
1. Urakami E. Differential diagnosis of tuberculosis: a relapse of tuberculosis in the early stage of chemotherapy. Kekkaku. 1982. 57:544–548.2. Sato H, Oizumi K, Motomiya M, Konno K. Reversible roentgenographic progression in the treatment of pulmonary tuberculosis. Kekkaku. 1982. 57:425–427.3. Onwubalili JK, Scott GM, Smith H. Acute respiratory distress related to chemotherapy of advanced pulmonary tuberculosis: a study of two cases and review of the literature. Q J Med. 1986. 59:599–610.4. Akira M, Sakatani M, Ishikawa H. Transient radiographic progression during initial treatment of pulmonary tuberculosis: CT findings. J Comput Assist Tomogr. 2000. 24:426–431.5. Lee CH, Kim WJ, Yoo CG, Kim YW, Han SK, Shim YS, et al. Response to empirical anti-tuberculosis treatment in patients with sputum smear-negative presumptive pulmonary tuberculosis. Respiration. 2005. 72:369–374.6. Iwai K, Kino C, Tsuchiya S, Kita R, Kinoshita T. Histological observation on the tuberculous lesions aggravated during rifampicin treatment. Kekkaku. 1979. 54:473–478.7. Bobrowitz ID. Reversible roentgenographic progression in the initial treatment of pulmonary tuberculosis. Am Rev Respir Dis. 1980. 121:735–742.8. Choi YW, Jeon SC, Seo HS, Park CK, Park SS, Hahm CK, et al. Tuberculous pleural effusion: new pulmonary lesions during treatment. Radiology. 2002. 224:493–502.9. Canetti G. Present aspects of bacterial resistance in tuberculosis. Am Rev Respir Dis. 1965. 92:687–703.10. Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, et al. American Thoracic Society/Center for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003. 167:603–662.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary paragonimiasis: CT findings
- Cystic Change in Pulmonary Tuberculosis in an Immunocompetent Adult: A Case Report
- Lobar Atelectasis: Typical and Atypical Radiographic and CT Findings
- Radiographic Findings of Pulmonary Tuberculosis in Non-AIDS Immunocompromised adult Patients: Comparison with Immunocompetent Adult Patients
- Radiographic Findings of Pulmonary Tuberculosis in Adult Diabetic Patients' Comparison of Diabetics with Nondiabetics of no Other Underlying Diseases