Korean J Urol.
2012 Nov;53(11):743-749.
Current Status of Brachytherapy for Prostate Cancer
- Affiliations
-
- 1Department of Urology, Bundang CHA Hospital, CHA University College of Medicine, Seongnam, Korea. dsparkmd@cha.ac.kr
Abstract
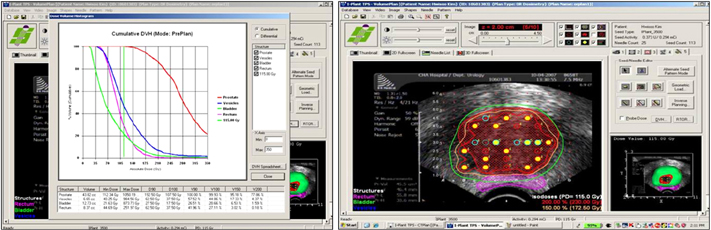
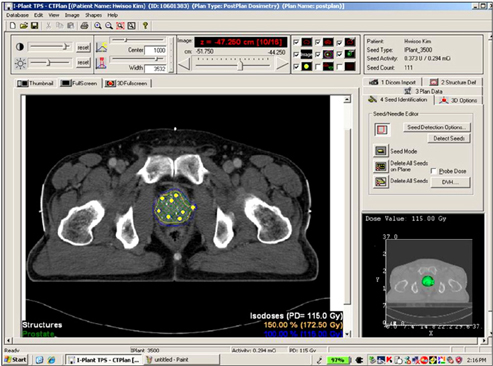
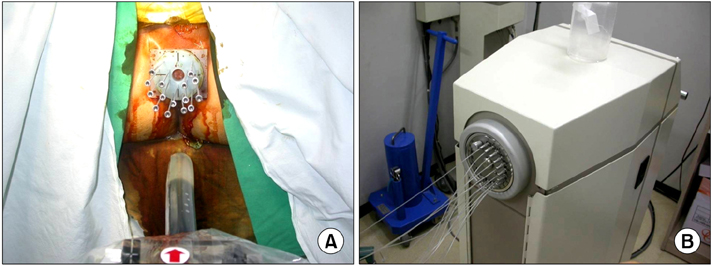
- Brachytherapy was developed to treat prostate cancer 50 years ago. Current advanced techniques using transrectal ultrasonography were established 25 years ago. Transrectal ultrasound (TRUS) has enabled the prostate to be viewed with improved resolution with the use of modern ultrasound machines. Moreover, the development of software that can provide images captured in real time has improved treatment outcomes. Other new radiologic imaging technologies or a combination of magnetic resonance and TRUS could be applied to brachytherapy in the future. The therapeutic value of brachytherapy for early-stage prostate cancer is comparable to that of radical prostatectomy in long-term follow-up. Nevertheless, widespread application of brachytherapy cannot be achieved for several reasons. The treatment outcome of brachytherapy varies according to the skill of the operator and differences in patient selection. Currently, only three radioactive isotopes are available for use in low dose rate prostate brachytherapy: I-125, Pd-103, and Cs-131; therefore, more isotopes should be developed. High dose rate brachytherapy using Ir-192 combined with external beam radiation, which is needed to verify the long-term effects, has been widely applied in high-risk patient groups. Recently, tumor-selective therapy or focal therapy using brachytherapy, which is not possible by surgical extraction, has been developed to maintain the quality of life in selected cases. However, this new application for prostate cancer treatment should be performed cautiously because we do not know the oncological outcome, and it would be an interim treatment method. This technique might evolve into a hybrid of whole-gland treatment and focal therapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Whitmore WF Jr, Hilaris B, Grabstald H. Retropubic implantation to iodine 125 in the treatment of prostatic cancer. J Urol. 1972. 108:918–920.2. Stamey TA, Caldwell M, McNeal JE, Nolley R, Hemenez M, Downs J. The prostate specific antigen era in the United States is over for prostate cancer: what happened in the last 20 years? J Urol. 2004. 172(4 Pt 1):1297–1301.3. Park DS, Jang WK, Oh JJ, Jee SH, Shin HS. Application of low dose rate brachytherapy in locally advanced prostate cancer. Korean J Urol Oncol. 2008. 6:127–132.4. Stock RG, Stone NN, Wesson MF, DeWyngaert JK. A modified technique allowing interactive ultrasound-guided three-dimensional transperineal prostate implantation. Int J Radiat Oncol Biol Phys. 1995. 32:219–225.5. Park DS, Oh JJ, Jang WK, Jee SH, Shin HS. Low-dose-rate brachytherapy for low- and intermediate-risk groups of localized prostate cancer. Korean J Urol. 2009. 50:656–662.6. Zelefsky MJ, Yamada Y, Cohen G, Venkatraman ES, Fung AY, Furhang E, et al. Postimplantation dosimetric analysis of permanent transperineal prostate implantation: improved dose distributions with an intraoperative computer-optimized conformal planning technique. Int J Radiat Oncol Biol Phys. 2000. 48:601–608.7. Yu Y, Anderson LL, Li Z, Mellenberg DE, Nath R, Schell MC, et al. Permanent prostate seed implant brachytherapy: report of the American Association of Physicists in Medicine Task Group No. 64. Med Phys. 1999. 26:2054–2076.8. Salembier C, Lavagnini P, Nickers P, Mangili P, Rijnders A, Polo A, et al. Tumour and target volumes in permanent prostate brachytherapy: a supplement to the ESTRO/EAU/EORTC recommendations on prostate brachytherapy. Radiother Oncol. 2007. 83:3–10.9. Merrick GS, Grimm PD, Sylvester J, Blasko JC, Butler WM, Allen ZA, et al. Initial analysis of Pro-Qura: a multi-institutional database of prostate brachytherapy dosimetry. Brachytherapy. 2007. 6:9–15.10. Lee WR, deGuzman AF, Tomlinson SK, McCullough DL. Radioactive sources embedded in suture are associated with improved postimplant dosimetry in men treated with prostate brachytherapy. Radiother Oncol. 2002. 65:123–127.11. Fagundes HM, Keys RJ, Wojcik MF, Radden MA, Bertelsman CG, Cavanagh WA. Transperineal TRUS-guided prostate brachytherapy using loose seeds versus RAPIDStrand: a dosimetric analysis. Brachytherapy. 2004. 3:136–140.12. Fuller DB, Koziol JA, Feng AC. Prostate brachytherapy seed migration and dosimetry: analysis of stranded sources and other potential predictive factors. Brachytherapy. 2004. 3:10–19.13. Heysek RV, Gwede CK, Torres-Roca J, Cantor A, Kelley S, Saini AS, et al. A dosimetric analysis of unstranded seeds versus customized stranded seeds in transperineal interstitial permanent prostate seed brachytherapy. Brachytherapy. 2006. 5:244–250.14. Reed DR, Wallner KE, Merrick GS, Arthurs S, Mueller A, Cavanagh W, et al. A prospective randomized comparison of stranded vs. loose 125I seeds for prostate brachytherapy. Brachytherapy. 2007. 6:129–134.15. Saibishkumar EP, Borg J, Yeung I, Cummins-Holder C, Landon A, Crook J. Sequential comparison of seed loss and prostate dosimetry of stranded seeds with loose seeds in 125I permanent implant for low-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2009. 73:61–68.16. Langley SE, Laing RW. 4D Brachytherapy, a novel real-time prostate brachytherapy technique using stranded and loose seeds. BJU Int. 2012. 109:Suppl 1. 1–6.17. Grimm PD, Blasko JC, Sylvester JE, Meier RM, Cavanagh W. 10-year biochemical (prostate-specific antigen) control of prostate cancer with (125)I brachytherapy. Int J Radiat Oncol Biol Phys. 2001. 51:31–40.18. Kollmeier MA, Stock RG, Stone N. Biochemical outcomes after prostate brachytherapy with 5-year minimal follow-up: importance of patient selection and implant quality. Int J Radiat Oncol Biol Phys. 2003. 57:645–653.19. Giberti C, Chiono L, Gallo F, Schenone M, Gastaldi E. Radical retropubic prostatectomy versus brachytherapy for low-risk prostatic cancer: a prospective study. World J Urol. 2009. 27:607–612.20. Fisher CM, Troncoso P, Swanson DA, Munsell MF, Kuban DA, Lee AK, et al. Knife or needles? A cohort analysis of outcomes after radical prostatectomy or brachytherapy for men with low- or intermediate-risk adenocarcinoma of the prostate. Brachytherapy. 2012. 11:429–434.21. Zelefsky MJ, Hollister T, Raben A, Matthews S, Wallner KE. Five-year biochemical outcome and toxicity with transperineal CT-planned permanent I-125 prostate implantation for patients with localized prostate cancer. Int J Radiat Oncol Biol Phys. 2000. 47:1261–1266.22. Merrick GS, Butler WM, Galbreath RW, Lief JH. Five-year biochemical outcome following permanent interstitial brachytherapy for clinical T1-T3 prostate cancer. Int J Radiat Oncol Biol Phys. 2001. 51:41–48.23. Kwok Y, DiBiase SJ, Amin PP, Naslund M, Sklar G, Jacobs SC. Risk group stratification in patients undergoing permanent (125)I prostate brachytherapy as monotherapy. Int J Radiat Oncol Biol Phys. 2002. 53:588–594.24. Kollmeier MA, Pei X, Algur E, Yamada Y, Cox BW, Cohen GN, et al. A comparison of the impact of isotope ((125)I vs. (103)Pd) on toxicity and biochemical outcome after interstitial brachytherapy and external beam radiation therapy for clinically localized prostate cancer. Brachytherapy. 2012. 11:271–276.25. Sylvester JE, Blasko JC, Grimm PD, Meier R, Malmgren JA. Ten-year biochemical relapse-free survival after external beam radiation and brachytherapy for localized prostate cancer: the Seattle experience. Int J Radiat Oncol Biol Phys. 2003. 57:944–952.26. Grimm P, Billiet I, Bostwick D, Dicker AP, Frank S, Immerzeel J, et al. Comparative analysis of prostate-specific antigen free survival outcomes for patients with low, intermediate and high risk prostate cancer treatment by radical therapy. Results from the Prostate Cancer Results Study Group. BJU Int. 2012. 109:Suppl 1. 22–29.27. Grimm PD, Blasko JC, Ragde H, Sylvester J, Clarke D. Does brachytherapy have a role in the treatment of prostate cancer? Hematol Oncol Clin North Am. 1996. 10:653–673.28. Locke J, Ellis W, Wallner K, Cavanagh W, Blasko J. Risk factors for acute urinary retention requiring temporary intermittent catheterization after prostate brachytherapy: a prospective study. Int J Radiat Oncol Biol Phys. 2002. 52:712–719.29. Crook J, McLean M, Catton C, Yeung I, Tsihlias J, Pintilie M. Factors influencing risk of acute urinary retention after TRUS-guided permanent prostate seed implantation. Int J Radiat Oncol Biol Phys. 2002. 52:453–460.30. Terk MD, Stock RG, Stone NN. Identification of patients at increased risk for prolonged urinary retention following radioactive seed implantation of the prostate. J Urol. 1998. 160:1379–1382.31. Emara AM, Chadwick E, Noves JP, Abdelbaky AM, Laing RW, Langley SE. Long-term toxicity and quality of life up to 10 years after low-dose rate brachytherapy for prostate cancer. BJU Int. 2012. 109:994–1000.32. Potters L, Torre T, Fearn PA, Leibel SA, Kattan MW. Potency after permanent prostate brachytherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2001. 50:1235–1242.33. Emara AM, Chadwick E, Nobes JP, Abdelbaky AM, Laing RW, Langley SE. Long-term toxicity and quality of life up to 10 years after low-dose rate brachytherapy for prostate cancer. BJU Int. 2012. 109:994–1000.34. Mate TP, Gottesman JE, Hatton J, Gribble M, Van Hollebeke L. High dose-rate afterloading 192Iridium prostate brachytherapy: feasibility report. Int J Radiat Oncol Biol Phys. 1998. 41:525–533.35. Dinges S, Deger S, Koswig S, Boehmer D, Schnorr D, Wiegel T, et al. High-dose rate interstitial with external beam irradiation for localized prostate cancer--results of a prospective trial. Radiother Oncol. 1998. 48:197–202.36. Hoskin PJ, Rojas AM, Bownes PJ, Lowe GJ, Ostler PJ, Bryant L. Randomised trial of external beam radiotherapy alone or combined with high-dose-rate brachytherapy boost for localised prostate cancer. Radiother Oncol. 2012. 103:217–222.37. Martinez AA, Gonzalez J, Ye H, Ghilezan M, Shetty S, Kernen K, et al. Dose escalation improves cancer-related events at 10 years for intermediate- and high-risk prostate cancer patients treated with hypofractionated high-dose-rate boost and external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2011. 79:363–370.38. Krishnamurthy D, Weinberg V, Cunha JA, Hsu IC, Pouliot J. Comparison of high-dose rate prostate brachytherapy dose distributions with iridium-192, ytterbium-169, and thulium-170 sources. Brachytherapy. 2011. 10:461–465.39. Langley S, Ahmed HU, Al-Qaisieh B, Bostwick D, Dickinson L, Veiga FG, et al. Report of a consensus meeting on focal low dose rate brachytherapy for prostate cancer. BJU Int. 2012. 109:Suppl 1. 7–16.