Korean J Urol.
2013 Feb;54(2):143-146.
Ileo-Pelvic Anastomosis and Augmentation Cystoplasty for Treatment of Encrusted Pyelitis in a Transplanted Kidney
- Affiliations
-
- 1Department of Urology, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. urosh@hanmail.net
- 2Department of Urology, Inje University Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
Abstract
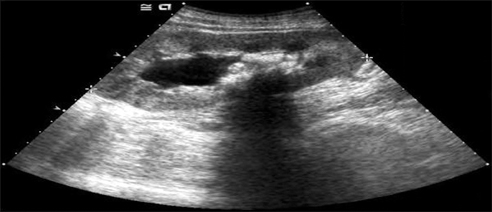
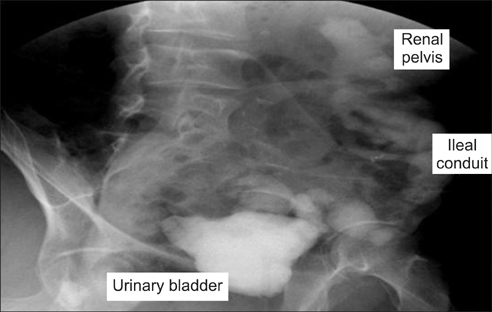
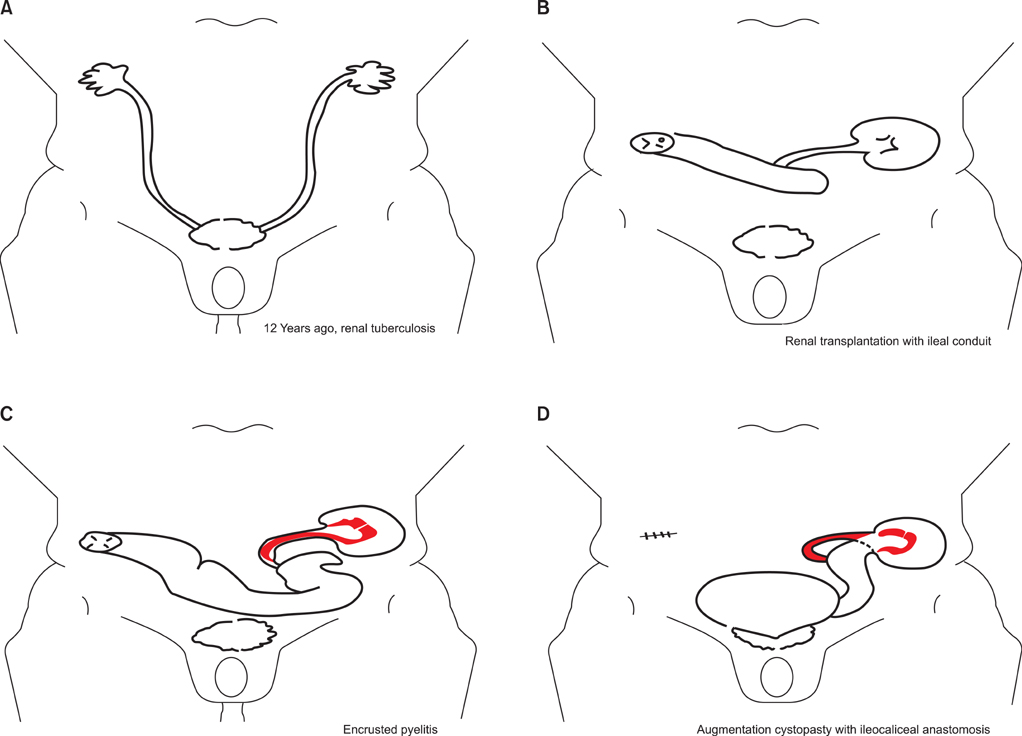
- Infection stones are more likely to form after urinary diversion as the result of urinary stasis. To prevent urinary stasis due to encrusted pyelitis in a transplanted kidney, we describe an alternative a surgical treatment: ileo-pelvic anastomosis. In our patient with a transplanted kidney, the ileal conduit had previously been anastomosed end-to-side owing to renal tuberculosis with an atrophied bladder; the transplanted ureter was anastomosed to the ileum in the left lower abdomen with an ileal conduit on the opposite side. Routine check-up revealed hydronephrosis with infected pyelitis and ureteritis in the transplanted kidney. We performed ileo-pelvic end-to-end anastomosis to prevent urinary stasis by lengthening the ileal conduit and performed augmentation cystoplasty to support the atrophied bladder following tuberculosis. We suggest that this approach may be useful in similar cases.
Keyword
MeSH Terms
Figure
Reference
-
1. Parmar MS. Kidney stones. BMJ. 2004. 328:1420–1424.2. Wong HY, Riedl CR, Griffith DP. Coe FL, Favus MJ, Pak CYC, Parks JH, Preminger GM, editors. Medical management and prevention of struvite stones. Kidney stones: medical and surgical management. 1996. Philadelphia: Lippincott-Raven;941–950.3. Meria P, Margaryan M, Haddad E, Dore B, Lottmann HB. Encrusted cystitis and pyelitis in children: an unusual condition with potentially severe consequences. Urology. 2004. 64:569–573.4. Benoit G, Eschwege P, Paradis V, Droupy S, Nordmann P, Charpentier B. Successful treatment of encrusted pyelitis in a renal transplant with local acidification and surgical ileocaliceal anastomosis. J Urol. 1999. 162:1369–1370.5. Stein RJ, Turna B, Patel NS, Weight CJ, Nguyen MM, Shah G, et al. Laparoscopic assisted ileal ureter: technique, outcomes and comparison to the open procedure. J Urol. 2009. 182:1032–1039.6. Gupta NP, Kumar A, Sharma S. Reconstructive bladder surgery in genitourinary tuberculosis. Indian J Urol. 2008. 24:382–387.7. Lee SS, Kang WG, Huh K, Kim DW, Kim GH, Shin YH, et al. Dysfunctional contracted bladder in renal transplantation. J Korean Soc Transplant. 2007. 21:257–261.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antirefluxing Augmentation Cystoplasty with Ileocolic Pouch in Single Kidney with Refluxing Contracted Bladder
- Functional Analysis of Anti-Refluxing Augmentation Cystoplasty
- A Case of Pyelitis and Ureteritis Cystica
- Augmentation Cystoplasty with Mainz Pouch in Tuberculous Contracted Bladder
- Renal transplantation in patients with an augmentation cystoplasty