Korean J Urol.
2013 Jun;54(6):373-376.
Functional Outcomes and Long-term Durability of Artificial Urinary Sphincter Application: Review of 56 Patients With Long-term Follow-up
- Affiliations
-
- 1Department of Urology, Ankara University Faculty of Medicine, Ankara, Turkey. migokce@yahoo.com
- 2Department of Urology, Ufuk University Faculty of Medicine, Ankara, Turkey.
Abstract
- PURPOSE
To evaluate the long-term outcomes of artificial urinary sphincter (AUS) implantation and to report the complication rates, including mechanical failure, erosion, and infection.
MATERIALS AND METHODS
From June 1990 to May 2011, AUS (AMS 800) implantations were performed in 56 adult males by one surgeon. Various demographic and preoperative variables, surgical variables, and postoperative outcomes, including success and complication rates with a median follow-up of 96 months, were recorded retrospectively.
RESULTS
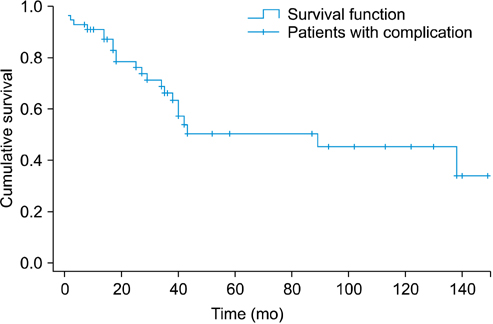
The mean age of the patients at the time of AUS implantation was 61.8 (+/-14.2) years. During the follow-up period, the total complication rate was 41.1% (23 patients). The incidence of complications was significantly lower during the follow-up period after 48 months (p<0.05). Kaplan-Meier analysis revealed that 5- and 10-year failure-free rates were 50.3% and 45.2%, respectively.
CONCLUSIONS
Long-term durability and functional outcomes are achievable for the AMS 800, but there are appreciable complication rates for erosion, mechanical failure, and infection of up to 30%.
MeSH Terms
Figure
Reference
-
1. Schroder A, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ, et al. Guidelines on urinary incontinence. In : Aus G, editor. EAU guidelines. Arnheim: European Association of Urology;2009. p. 11–28.2. Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008; 358:1250–1261.3. Benoit RM, Naslund MJ, Cohen JK. Complications after radical retropubic prostatectomy in the medicare population. Urology. 2000; 56:116–120.4. Fishman IJ, Shabsigh R, Scott FB. Experience with the artificial urinary sphincter model AS800 in 148 patients. J Urol. 1989; 141:307–310.5. Lee R, Te AE, Kaplan SA, Sandhu JS. Temporal trends in adoption of and indications for the artificial urinary sphincter. J Urol. 2009; 181:2622–2627.6. Haab F, Trockman BA, Zimmern PE, Leach GE. Quality of life and continence assessment of the artificial urinary sphincter in men with minimum 3.5 years of followup. J Urol. 1997; 158:435–439.7. Kim SP, Sarmast Z, Daignault S, Faerber GJ, McGuire EJ, Latini JM. Long-term durability and functional outcomes among patients with artificial urinary sphincters: a 10-year retrospective review from the University of Michigan. J Urol. 2008; 179:1912–1916.8. Fulford SC, Sutton C, Bales G, Hickling M, Stephenson TP. The fate of the 'modern' artificial urinary sphincter with a follow-up of more than 10 years. Br J Urol. 1997; 79:713–716.9. Gousse AE, Madjar S, Lambert MM, Fishman IJ. Artificial urinary sphincter for post-radical prostatectomy urinary incontinence: long-term subjective results. J Urol. 2001; 166:1755–1758.10. Montague DK, Angermeier KW, Paolone DR. Long-term continence and patient satisfaction after artificial sphincter implantation for urinary incontinence after prostatectomy. J Urol. 2001; 166:547–549.11. Elliott DS, Barrett DM. Mayo Clinic long-term analysis of the functional durability of the AMS 800 artificial urinary sphincter: a review of 323 cases. J Urol. 1998; 159:1206–1208.12. Lai HH, Hsu EI, Teh BS, Butler EB, Boone TB. 13 years of experience with artificial urinary sphincter implantation at Baylor College of Medicine. J Urol. 2007; 177:1021–1025.13. Trigo Rocha F, Gomes CM, Mitre AI, Arap S, Srougi M. A prospective study evaluating the efficacy of the artificial sphincter AMS 800 for the treatment of postradical prostatectomy urinary incontinence and the correlation between preoperative urodynamic and surgical outcomes. Urology. 2008; 71:85–89.14. Walsh IK, Williams SG, Mahendra V, Nambirajan T, Stone AR. Artificial urinary sphincter implantation in the irradiated patient: safety, efficacy and satisfaction. BJU Int. 2002; 89:364–368.15. Thiel DD, Young PR, Broderick GA, Heckman MG, Wehle MJ, Igel TC, et al. Do clinical or urodynamic parameters predict artificial urinary sphincter outcome in post-radical prostatectomy incontinence? Urology. 2007; 69:315–319.16. Arai Y, Kaiho Y, Takei M, Nonomura K, Baba S, Habuchi T, et al. Burden of male stress urinary incontinence: a survey among urologists in Japan. Int J Urol. 2009; 16:915–917.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reimbursement for the Long-Term Care
- Long Term Follow-up Results of Anterior Vaginal Wall Sling Procedure for Female Stress Urinary Incontinence
- Long-term Outcome of the Readjustable Sling Procedure for Female Stress Urinary Incontinence With Intrinsic Sphincter Deficiency or Recurrence
- Long-term follow-up study and long-term care of childhood cancer survivors
- Long-Term Care System in Korea