J Korean Neurosurg Soc.
2016 Jul;59(4):357-362. 10.3340/jkns.2016.59.4.357.
Meningiomas with Rhabdoid or Papillary Components : Prognosis and Comparison with Anaplastic Meningiomas
- Affiliations
-
- 1Department of Neurosurgery, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Gwangju, Korea. jung-ty@chonnam.ac.kr
- 2Department of Pathology, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Gwangju, Korea.
- 3Department of Radiology, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Gwangju, Korea.
- 4Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2315970
- DOI: http://doi.org/10.3340/jkns.2016.59.4.357
Abstract
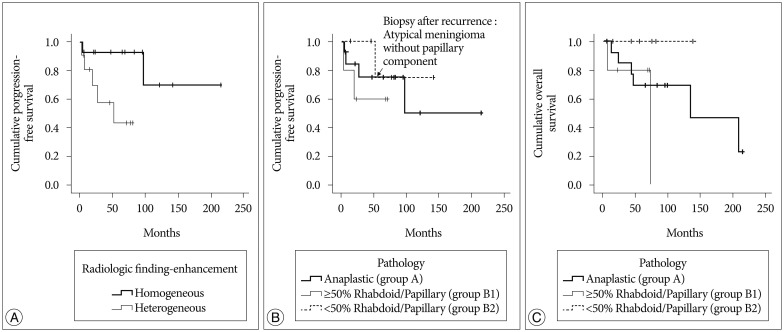
- Papillary and rhabdoid meningiomas are pathologically World Health Organization (WHO) grade III. Any correlation between clinical prognosis and pathologic component is not clear. We analyzed the prognoses of patients with meningiomas with a rhabdoid or papillary component compared to those of patients with anaplastic meningiomas. From 1994 to June 2013, 14 anaplastic meningiomas, 6 meningiomas with a rhabdoid component, and 5 meningiomas with papillary component were pathologically diagnosed. We analyzed magnetic resonance imaging (MRI) findings, extent of removal, adjuvant treatment, progression-free survival (PFS), overall survival (OS), and pathologic features of 14 anaplastic meningiomas (group A), 5 meningiomas with a predominant (≥50%) papillary or rhabdoid component (group B1), and 6 meningiomas without a predominant (<50%) rhabdoid or papillary component (group B2). Homogeneous enhancement on MRI was associated with improved PFS compared to heterogeneous enhancement (p=0.025). Depending on pathology, the mean PFS was 134.9±31.6 months for group A, 46.6±13.4 months for group B1, and 118.7±19.2 months for group B2. The mean OS was 138.5±24.6 months for group A and 59.7±16.8 months for group B1. All recurrent tumors were of the previously diagnosed pathology, except for one tumor from group B1, which recurred as an atypical meningioma without a papillary component. Group B1 tumors showed a more aggressive behavior than group B2 tumors. In group B2 cases, the pathologic findings of non-rhabdoid/papillary portion could be considered for further adjuvant treatment.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Anaplastic Meningioma: Clinical Characteristics, Prognostic Factors and Survival Outcome
Dong Ok Seo, Sang Woo Song, Young-Hoon Kim, Chang-Ki Hong, Jeong Hoon Kim
Brain Tumor Res Treat. 2022;10(4):244-254. doi: 10.14791/btrt.2022.0030.
Reference
-
1. Al-Habib A, Lach B, Al Khani A. Intracerebral rhabdoid and papillary meningioma with leptomeningeal spread and rapid clinical progression. Clin Neuropathol. 2005; 24:1–7. PMID: 15696777.2. Durand A, Labrousse F, Jouvet A, Bauchet L, Kalamaridès M, Menei P, et al. WHO grade II and III meningiomas : a study of prognostic factors. J Neurooncol. 2009; 95:367–375. PMID: 19562258.
Article3. Hug EB, Devries A, Thornton AF, Munzenride JE, Pardo FS, Hedley-Whyte ET, et al. Management of atypical and malignant meningiomas : role of high-dose, 3D-conformal radiation therapy. J Neurooncol. 2000; 48:151–160. PMID: 11083080.4. Karabagli P, Karabagli H, Yavas G. Aggressive rhabdoid meningioma with osseous, papillary and chordoma-like appearance. Neuropathology. 2014; 34:475–483. PMID: 24702318.
Article5. Kasuya H, Kubo O, Tanaka M, Amano K, Kato K, Hori T. Clinical and radiological features related to the growth potential of meningioma. Neurosurg Rev. 2006; 29:293–296. discussion 296-297. PMID: 16953450.
Article6. Kepes JJ, Moral LA, Wilkinson SB, Abdullah A, Llena JF. Rhabdoid transformation of tumor cells in meningiomas : a histologic indication of increased proliferative activity : report of four cases. Am J Surg Pathol. 1998; 22:231–238. PMID: 9500225.7. Kim JP, Park BJ, Lim YJ. Papillary meningioma with leptomeningeal seeding. J Korean Neurosurg Soc. 2011; 49:124–127. PMID: 21519503.
Article8. Kliese N, Gobrecht P, Pachow D, Andrae N, Wilisch-Neumann A, Kirches E, et al. miRNA-145 is downregulated in atypical and anaplastic meningiomas and negatively regulates motility and proliferation of meningioma cells. Oncogene. 2013; 32:4712–4720. PMID: 23108408.
Article9. Koenig MA, Geocadin RG, Kulesza P, Olivi A, Brem H. Rhabdoid meningioma occurring in an unrelated resection cavity with leptomeningeal carcinomatosis. Case report. J Neurosurg. 2005; 102:371–375. PMID: 15739568.
Article10. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK. WHO Classification of tumours of the central nervous system. ed 3. Lyon: IARC;2007. p. 164–172.11. Mahmood A, Caccamo DV, Tomecek FJ, Malik GM. Atypical and malignant meningiomas : a clinicopathological review. Neurosurgery. 1993; 33:955–963. PMID: 8134008.12. Milosevic MF, Frost PJ, Laperriere NJ, Wong CS, Simpson WJ. Radiotherapy for atypical or malignant intracranial meningioma. Int J Radiat Oncol Biol Phys. 1996; 34:817–822. PMID: 8598358.
Article13. Modha A, Gutin PH. Diagnosis and treatment of atypical and anaplastic meningiomas : a review. Neurosurgery. 2005; 57:538–550. discussion 538-550. PMID: 16145534.
Article14. Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982; 5:649–655. PMID: 7165009.
Article15. Rogerio F, de Araújo Zanardi V, Ribeiro de Menezes Netto J, de Souza Queiroz L. Meningioma with rhabdoid, papillary and clear cell features : case report and review of association of rare meningioma variants. Clin Neuropathol. 2011; 30:291–296. PMID: 22011733.
Article16. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957; 20:22–39. PMID: 13406590.
Article17. Sun SQ, Hawasli AH, Huang J, Chicoine MR, Kim AH. An evidence-based treatment algorithm for the management of WHO Grade II and III meningiomas. Neurosurg Focus. 2015; 38:E3. PMID: 25727225.
Article18. Verheggen R, Finkenstaedt M, Bockermann V, Markakis E. Atypical and malignant meningiomas : evaluation of different radiological criteria based on CT and MRI. Acta Neurochir Suppl. 1996; 65:66–69. PMID: 8738499.19. Vinchon M, Ruchoux MM, Lejeune JP, Assaker R, Christiaens JL. Carcinomatous meningitis in a case of anaplastic meningioma. J Neurooncol. 1995; 23:239–243. PMID: 7673986.
Article20. Wu YT, Ho JT, Lin YJ, Lin JW. Rhabdoid papillary meningioma : a clinicopathologic case series study. Neuropathology. 2011; 31:599–605. PMID: 21382093.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Loss of Heterozygosity at 1p, 7q, 17p, and 22q in Meningiomas
- Multiple Meningiomas: A Case Report
- Multiple Intracranial Meningiomas: Case Report
- Correlation between Expression of p53 Protein and Prognostic Factors in Meningiomas
- A Study of AgNORs(Argyrophilic Nucleolar Organizer Regions) on Prediction of the Prognosis in Intracranial Meningiomas