J Korean Neurosurg Soc.
2016 Jul;59(4):346-351. 10.3340/jkns.2016.59.4.346.
Perfusion-Weighted MRI Parameters for Prediction of Early Progressive Infarction in Middle Cerebral Artery Occlusion
- Affiliations
-
- 1Department of Neurosurgery, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
- 2Department of Neurology, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
- 3Department of Neurosurgery, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea. 72ysh@catholic.ac.kr
- KMID: 2315968
- DOI: http://doi.org/10.3340/jkns.2016.59.4.346
Abstract
OBJECTIVE
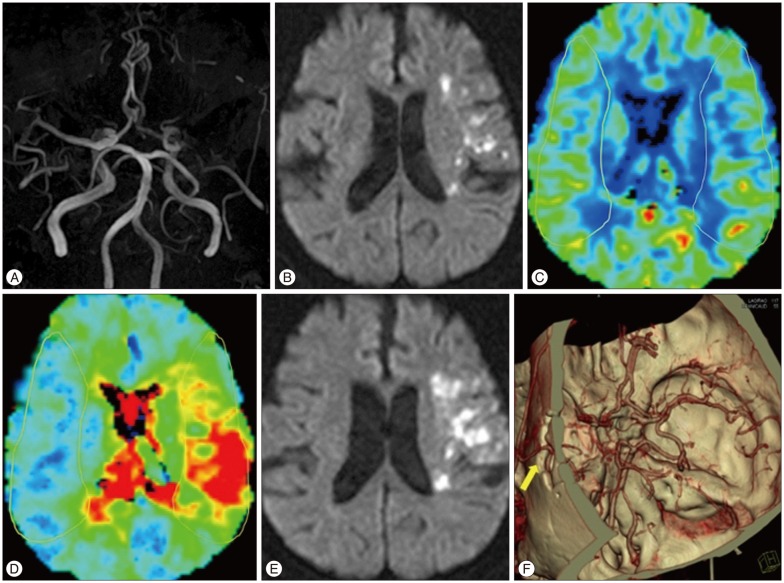
Early progressive infarction (EPI) is frequently observed and related to poor functional outcome in patients with middle cerebral artery (MCA) infarction caused by MCA occlusion. We evaluated the perfusion parameters of magnetic resonance imaging (MRI) as a predictor of EPI.
METHODS
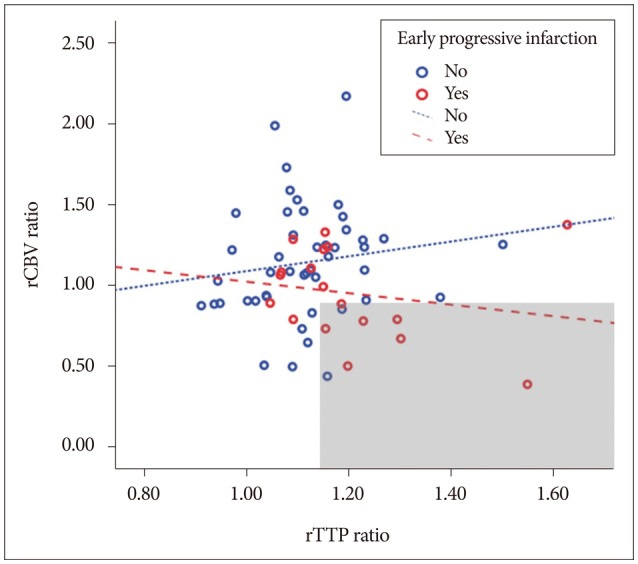
We retrospectively analyzed patients with acute MCA territory infarction caused by MCA occlusion. EPI was defined as a National Institutes of Health Stroke Scale increment ≥2 points during 24 hours despite receiving standard treatment. Regional parameter ratios, such as cerebral blood flow and volume (rCBV) ratio (ipsilateral value/contralateral value) on perfusion MRI were analyzed to investigate the association with EPI.
RESULTS
Sixty-four patients were enrolled in total. EPI was present in 18 (28%) subjects and all EPI occurred within 3 days after hospitalization. Diabetes mellitus, rCBV ratio and regional time to peak (rTTP) ratio showed statically significant differences in both groups. Multi-variate analysis indicated that history of diabetes mellitus [odds ratio (OR), 6.13; 95% confidence interval (CI), 1.55-24.24] and a low rCBV ratio (rCBV, <0.85; OR, 6.57; 95% CI, 1.4-30.27) was significantly correlated with EPI.
CONCLUSION
The incidence of EPI is considerable in patients with acute MCA territory infarction caused by MCA occlusion. We suggest that rCBV ratio is a useful neuro-imaging parameter to predict EPI.
Keyword
MeSH Terms
Figure
Reference
-
1. Alawneh JA, Moustafa RR, Baron JC. Hemodynamic factors and perfusion abnormalities in early neurological deterioration. Stroke. 2009; 40:e443–e450. PMID: 19390076.
Article2. Birschel P, Ellul J, Barer D. Progressing stroke : towards an internationally agreed definition. Cerebrovasc Dis. 2004; 17:242–252. PMID: 14718754.
Article3. Campbell BC, Christensen S, Levi CR, Desmond PM, Donnan GA, Davis SM, et al. Cerebral blood flow is the optimal CT perfusion parameter for assessing infarct core. Stroke. 2011; 42:3435–3440. PMID: 21980202.
Article4. Campbell BC, Christensen S, Tress BM, Churilov L, Desmond PM, Parsons MW, et al. Failure of collateral blood flow is associated with infarct growth in ischemic stroke. J Cereb Blood Flow Metab. 2013; 33:1168–1172. PMID: 23652626.
Article5. Dávalos A, Cendra E, Teruel J, Martinez M, Genís D. Deteriorating ischemic stroke : risk factors and prognosis. Neurology. 1990; 40:1865–1869. PMID: 2247235.6. Desilles JP, Meseguer E, Labreuche J, Lapergue B, Sirimarco G, Gonzalez-Valcarcel J, et al. Diabetes mellitus, admission glucose, and outcomes after stroke thrombolysis : a registry and systematic review. Stroke. 2013; 44:1915–1923. PMID: 23704108.
Article7. Eusebi P. Diagnostic accuracy measures. Cerebrovasc Dis. 2013; 36:267–272. PMID: 24135733.
Article8. Hjalmarsson C, Manhem K, Bokemark L, Andersson B. The role of prestroke glycemic control on severity and outcome of acute ischemic stroke. Stroke Res Treat. 2014; 2014:694569. PMID: 25295219.
Article9. Horiuchi T, Nitta J, Ishizaka S, Kanaya K, Yanagawa T, Hongo K. Emergency EC-IC bypass for symptomatic atherosclerotic ischemic stroke. Neurosurg Rev. 2013; 36:559–564. discussion 564-565. PMID: 23821132.
Article10. Hou Q, Zuo Z, Michel P, Zhang Y, Eskandari A, Man F, et al. Influence of chronic hyperglycemia on cerebral microvascular remodeling : an in vivo study using perfusion computed tomography in acute ischemic stroke patients. Stroke. 2013; 44:3557–3560. PMID: 24029632.
Article11. Jia Q, Zhao X, Wang C, Wang Y, Yan Y, Li H, et al. Diabetes and poor outcomes within 6 months after acute ischemic stroke : the China National Stroke Registry. Stroke. 2011; 42:2758–2762. PMID: 21852614.
Article12. Jørgensen HS, Nakayama H, Raaschou HO, Olsen TS. Effect of blood pressure and diabetes on stroke in progression. Lancet. 1994; 344:156–159. PMID: 7912765.
Article13. Kawai N, Keep RF, Betz AL. Hyperglycemia and the vascular effects of cerebral ischemia. Acta Neurochir Suppl. 1997; 70:27–29. PMID: 9416268.
Article14. Khatri R, Rodriguez GJ, Suri MF, Vazquez G, Ezzeddine MA. Lepto meningeal collateral response and computed tomographic perfusion mismatch in acute middle cerebral artery occlusion. J Vasc Interv Neurol. 2011; 4:1–4. PMID: 22518259.15. Kimura K, Sakamoto Y, Iguchi Y, Shibazaki K, Aoki J, Sakai K, et al. Admission hyperglycemia and serial infarct volume after t-PA therapy in patients with and without early recanalization. J Neurol Sci. 2011; 307:55–59. PMID: 21624623.
Article16. Kluytmans M, van Everdingen KJ, Kappelle LJ, Ramos LM, Viergever MA, van der. Prognostic value of perfusion- and diffusion-weighted MR imaging in first 3 days of stroke. Eur Radiol. 2000; 10:1434–1441. PMID: 10997432.
Article17. Kwan J, Hand P. Early neurological deterioration in acute stroke : clinical characteristics and impact on outcome. QJM. 006; 99:625–633. PMID: 16905751.
Article18. Lee SB, Huh PW, Kim DS, Yoo DS, Lee TG, Cho KS. Early superficial temporal artery to middle cerebral artery bypass in acute ischemic stroke. Clin Neurol Neurosurg. 2013; 115:1238–1244. PMID: 23266265.
Article19. Lee SY, Cha JK, Kang MJ. Regional cerebral blood volume ratio on perfusion MRI on the growth of infarct size in acute ischemic stroke. Eur Neurol. 2009; 62:281–286. PMID: 19690421.
Article20. Lemkes BA, Hermanides J, Devries JH, Holleman F, Meijers JC, Hoekstra JB. Hyperglycemia : a prothrombotic factor? J Thromb Haemost. 2010; 8:1663–1669. PMID: 20492456.21. Liu Y, Karonen JO, Vanninen RL, Nuutinen J, Koskela A, Soimakallio S, et al. Acute ischemic stroke : predictive value of 2D phase-contrast MR angiography--serial study with combined diffusion and perfusion MR imaging. Radiology. 2004; 231:517–527. PMID: 15044743.
Article22. Neumann-Haefelin T, Wittsack HJ, Fink GR, Wenserski F, Li TQ, Seitz RJ, et al. Diffusion- and perfusion-weighted MRI : influence of severe carotid artery stenosis on the DWI/PWI mismatch in acute stroke. Stroke. 2000; 31:1311–1317. PMID: 10835450.23. Nussbaum ES, Janjua TM, Defillo A, Lowary JL, Nussbaum LA. Emergency extracranial-intracranial bypass surgery for acute ischemic stroke. J Neurosurg. 2010; 112:666–673. PMID: 19499983.
Article24. Reeves MJ, Vaidya RS, Fonarow GC, Liang L, Smith EE, Matulonis R, et al. Quality of care and outcomes in patients with diabetes hospitalized with ischemic stroke : findings from Get With the Guidelines-Stroke. Stroke. 2010; 41:e409–e417. PMID: 20224058.25. Schaefer PW, Hunter GJ, He J, Hamberg LM, Sorensen AG, Schwamm LH, et al. Predicting cerebral ischemic infarct volume with diffusion and perfusion MR imaging. AJNR Am J Neuroradiol. 2002; 23:1785–1794. PMID: 12427640.26. Schaefer PW, Souza L, Kamalian S, Hirsch JA, Yoo AJ, Kamalian S, et al. Limited reliability of computed tomographic perfusion acute infarct volume measurements compared with diffusion-weighted imaging in anterior circulation stroke. Stroke. 2015; 46:419–424. PMID: 25550366.
Article27. Seners P, Turc G, Oppenheim C, Baron JC. Incidence, causes and predictors of neurological deterioration occurring within 24 h following acute ischaemic stroke : a systematic review with pathophysiological implications. J Neurol Neurosurg Psychiatry. 2015; 86:87–94. PMID: 24970907.
Article28. Shimoyama T, Shibazaki K, Kimura K, Uemura J, Shiromoto T, Watanabe M, et al. Admission hyperglycemia causes infarct volume expansion in patients with ICA or MCA occlusion : association of collateral grade on conventional angiography. Eur J Neurol. 2013; 20:109–116. PMID: 22747888.
Article29. Srinivasan A, Goyal M, Al Azri F, Lum C. State-of-the-art imaging of acute stroke. Radiographics. 2006; 26(Suppl 1):S75–S95. PMID: 17050521.
Article30. Toni D, Fiorelli M, Gentile M, Bastianello S, Sacchetti ML, Argentino C, et al. Progressing neurological deficit secondary to acute ischemic stroke. A study on predictability, pathogenesis, and prognosis. Arch Neurol. 1995; 52:670–675. PMID: 7619022.
Article31. Toyoda K, Fujimoto S, Kamouchi M, Iida M, Okada Y. Acute blood pressure levels and neurological deterioration in different subtypes of ischemic stroke. Stroke. 2009; 40:2585–2588. PMID: 19407233.
Article32. Vaidyula VR, Rao AK, Mozzoli M, Homko C, Cheung P, Boden G. Effects of hyperglycemia and hyperinsulinemia on circulating tissue factor procoagulant activity and platelet CD40 ligand. Diabetes. 2006; 55:202–208. PMID: 16380494.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serial Magnetic Resonance Images of a Right Middle Cerebral Artery Infarction : Persistent Hyperintensity on Diffusion-Weighted MRI Over 8 Months
- Intracranial Cerebrovascular Revascularization(Extracranial-Intracranial Arterial Bypass, EIAB)
- Progressive Middle Cerebral Artery Infarction in a Patient with Thrombotic Thrombocytopenic Purpura
- Sphenoid Ridge Meningioma Presenting as Acute Cerebral Infarction
- The rCBV Ratio Is a Predictive Factor for Developing Malignant Middle Cerebral Artery Infarction within 6 Hours of Symptom Onset