Korean J Urol.
2009 Nov;50(11):1083-1088.
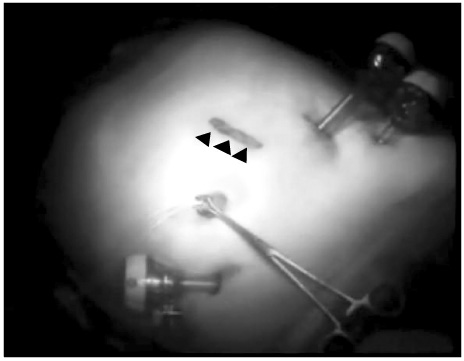
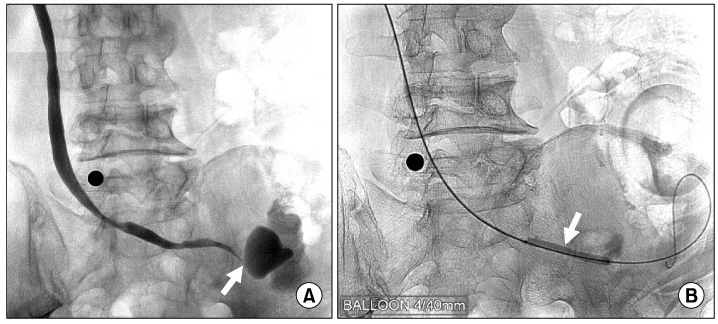
Short Term Comparative Analysis of Laparoscopic and Open Radical Cystectomy with Extracorporeal Urinary Diversion
- Affiliations
-
- 1Department of Urology, Sungkyunkwan University School of Medicine, Seoul, Korea. seongil.seo@samsung.com
Abstract
- PURPOSE
We analyzed the efficacy and safety of laparoscopic radical cystectomy (LRC) compared with open radical cystectomy (ORC).
MATERIALS AND METHODS
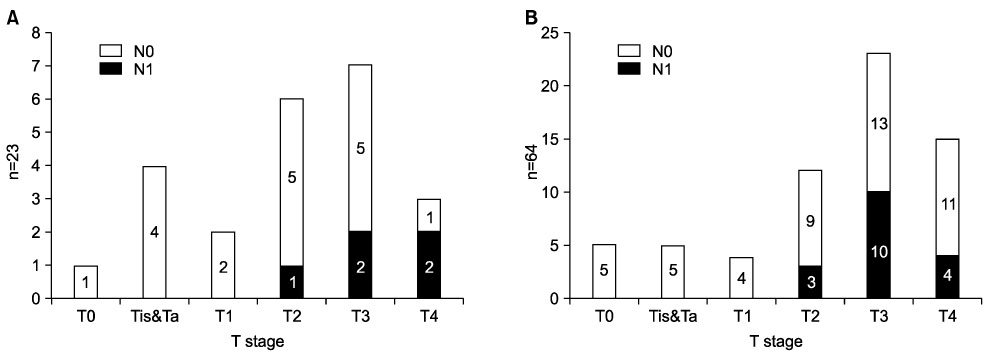
Between November 2007 and April 2009, we performed LRC to treat bladder cancer in 23 patients and ORC in 64 patients. Data including the patients' clinical characteristics, peri-operative parameters, clinical outcomes, and oncologic outcomes were collected retrospectively and analyzed by use of the Mann-Whitney U test and chi-square test.
RESULTS
There were no significant differences in demographic data between the two groups. Operative time was longer (595.2 min vs. 453.1 min; p<0.01) in the LRC group but blood loss was less (634.8 ml vs. 1,415.9 ml; p<0.01) and fewer transfusions were required (13.0% vs. 50.0%; p=0.002) in the LRC group. Days to oral intake (5.7 days vs. 7.3 days; p<0.01), days to drain removal (10.9 days vs. 13.9 days; p=0.014), and length of hospital stay (15.2 days vs. 22.3 days; p<0.01) were shorter in the LRC group. Postoperative complications occurred in 4 cases in the LRC group and 28 cases in the ORC group (17.4% vs. 43.8%, p<0.01). There were no cases with a positive surgical margin in the LRC group and 3 cases in the ORC group. There was no significant difference in the number of lymph nodes excised (17.4 vs. 19.6; p=0.132) between groups.
CONCLUSIONS
These short-term clinical and oncological results suggest that LRC is a safe and effective method for the treatment of invasive bladder cancer.
Keyword
MeSH Terms
Figure
Reference
-
1. Raychaudhuri B, Khan MS, Challacombe B, Rimington P, Dasgupta P. Minimally invasive radical cystectomy. BJU Int. 2006. 98:1064–1067.2. Bracken RB, McDonald M, Johnson DE. Complications of single-stage radical cystectomy and ileal conduit. Urology. 1981. 17:141–146.3. Terry WJ, Bueschen AJ. Complications of radical cystectomy and correlation with nutritional assessment. Urology. 1986. 27:229–232.4. Abdel-Hakim AM, Bassiouny F, Abdel Azim MS, Rady I, Mohey T, Habib I, et al. Laparoscopic radical cystectomy with orthotopic neobladder. J Endourol. 2002. 16:377–381.5. Gill IS, Fergany A, Klein EA, Kaouk JH, Sung GT, Meraney AM, et al. Laparoscopic radical cystoprostatectomy with ileal conduit performed completely intracorporeally: the initial 2 cases. Urology. 2000. 56:26–29.6. Simonato A, Gregori A, Lissiani A, Bozzola A, Galli S, Gaboardi F. Laparoscopic radical cystoprostatectomy: our experience in a consecutive series of 10 patients with a 3 years follow-up. Eur Urol. 2005. 47:785–790.7. Sanchez de Badajoz E, Gallego Perales JL, Reche Rosado A, Gutierrez de la Cruz JM, Jimenez Garrido A. Laparoscopic cystectomy and ileal conduit: case report. J Endourol. 1995. 9:59–62.8. Sung GT, Cho WY, Kim DW, Choi DW, Kim SD, Hwang JS, et al. Laparoscopic radical cystectomy with extracorporeal ileal conduit diversion. Korean J Urol. 2003. 44:826–831.9. Basillote JB, Abdelshehid C, Ahlering TE, Shanberg AM. Laparoscopic assisted radical cystectomy with ileal neobladder: a comparison with the open approach. J Urol. 2004. 172:489–493.10. Kwak JJ, Kim TH, Sung GT. Short term outcomes of laparoscopic radical cystectomy with an extracorporeal ileal conduit: comparative analysis with the open method. Korean J Urol. 2007. 48:938–944.11. Vallancien G, Abou El Fettouh H, Cathelineau X, Baumert H, Fromont G, Guillonneau B. Cystectomy with prostate sparing for bladder cancer in 100 patients: 10-year experience. J Urol. 2002. 168:2413–2417.12. Cathelineau X, Jaffe J. Laparoscopic radical cystectomy with urinary diversion: What is the optimal technique? Curr Opin Urol. 2007. 17:93–97.13. Hemal AK, Kolla SB, Wadhwa P, Dogra PN, Gupta NP. Laparoscopic radical cystectomy and extracorporeal urinary diversion: a single center experience of 48 cases with three years of follow-up. Urology. 2008. 71:41–46.14. Huang J, Lin T, Xu K, Huang H, Jiang C, Han J, et al. Laparoscopic radical cystectomy with orthotopic ileal neobladder: a report of 85 cases. J Endourol. 2008. 22:939–946.15. Honma I, Masumori N, Sato E, Maeda T, Hirobe M, Kitamura H, et al. Removal of more lymph nodes may provide better outcome, as well as more accurate pathologic findings, in patients with bladder cancer--analysis of role of pelvic lymph node dissection. Urology. 2006. 68:543–548.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robot-Assisted Laparoscopic Radical Cystectomy
- Laparoscopic Radical Cystectomy with Orthotopic Ileal W-neobladder
- Short Term Outcomes of Laparoscopic Radical Cystectomy with an Extracorporeal Ileal Conduit: Comparative Analysis with the Open Method
- Functional Outcomes and Quality of Life after Orthotopic Bladder Substitution in Bladder Cancer Patients
- Initial Experiences with Robot-Assisted Laparoscopic Radical Cystectomy