Obstet Gynecol Sci.
2014 Nov;57(6):427-435. 10.5468/ogs.2014.57.6.427.
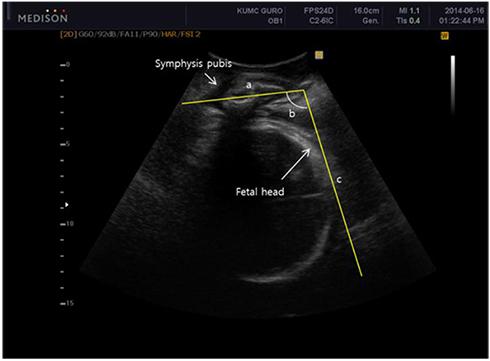
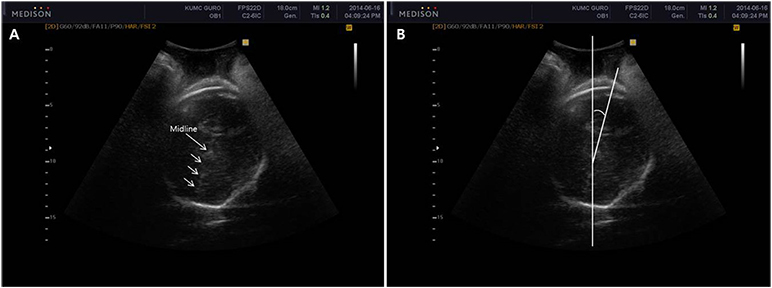
Intrapartum ultrasound: A useful method for evaluating labor progress and predicting operative vaginal delivery
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Korea University College of Medicine, Seoul, Korea. mjohmd@korea.ac.kr
- KMID: 2314007
- DOI: http://doi.org/10.5468/ogs.2014.57.6.427
Abstract
- The last step of a successful pregnancy is the safe delivery of the fetus. An important question is if the delivery should vaginal or operative. In addition to the use of conventional antenatal ultrasound, the use of intrapartum ultrasound to evaluate fetal head station, position, cervical ripening, and placental separation is promising. This review evaluates and summarizes the usefulness of intrapartum ultrasound for the evaluation of labor progress and predicting successful operative vaginal delivery.
Keyword
MeSH Terms
Figure
Reference
-
1. Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999; 341:1709–1714.2. Akmal S, Tsoi E, Kametas N, Howard R, Nicolaides KH. Intrapartum sonography to determine fetal head position. J Matern Fetal Neonatal Med. 2002; 12:172–177.3. Sherer DM, Miodovnik M, Bradley KS, Langer O. Intrapartum fetal head position II: comparison between transvaginal digital examination and transabdominal ultrasound assessment during the second stage of labor. Ultrasound Obstet Gynecol. 2002; 19:264–268.4. Sherer DM, Miodovnik M, Bradley KS, Langer O. Intrapartum fetal head position I: comparison between transvaginal digital examination and transabdominal ultrasound assessment during the active stage of labor. Ultrasound Obstet Gynecol. 2002; 19:258–263.5. Akmal S, Tsoi E, Howard R, Osei E, Nicolaides KH. Investigation of occiput posterior delivery by intrapartum sonography. Ultrasound Obstet Gynecol. 2004; 24:425–428.6. Cheng YW, Shaffer BL, Caughey AB. Associated factors and outcomes of persistent occiput posterior position: a retrospective cohort study from 1976 to 2001. J Matern Fetal Neonatal Med. 2006; 19:563–568.7. Blasi I, D'Amico R, Fenu V, Volpe A, Fuchs I, Henrich W, et al. Sonographic assessment of fetal spine and head position during the first and second stages of labor for the diagnosis of persistent occiput posterior position: a pilot study. Ultrasound Obstet Gynecol. 2010; 35:210–215.8. Gardberg M, Laakkonen E, Salevaara M. Intrapartum sonography and persistent occiput posterior position: a study of 408 deliveries. Obstet Gynecol. 1998; 91(5 Pt 1):746–749.9. Malvasi A, Stark M, Ghi T, Farine D, Guido M, Tinelli A. Intrapartum sonography for fetal head asynclitism and transverse position: sonographic signs and comparison of diagnostic performance between transvaginal and digital examination. J Matern Fetal Neonatal Med. 2012; 25:508–512.10. Malvasi A, Tinelli A, Brizzi A, Guido M, Laterza F, De Nunzio G, et al. Intrapartum sonography head transverse and asynclitic diagnosis with and without epidural analgesia initiated early during the first stage of labor. Eur Rev Med Pharmacol Sci. 2011; 15:518–523.11. Dupuis O, Silveira R, Zentner A, Dittmar A, Gaucherand P, Cucherat M, et al. Birth simulator: reliability of transvaginal assessment of fetal head station as defined by the American College of Obstetricians and Gynecologists classification. Am J Obstet Gynecol. 2005; 192:868–874.12. Eggebo TM, Gjessing LK, Heien C, Smedvig E, Okland I, Romundstad P, et al. Prediction of labor and delivery by transperineal ultrasound in pregnancies with prelabor rupture of membranes at term. Ultrasound Obstet Gynecol. 2006; 27:387–391.13. Barbera AF, Pombar X, Perugino G, Lezotte DC, Hobbins JC. A new method to assess fetal head descent in labor with transperineal ultrasound. Ultrasound Obstet Gynecol. 2009; 33:313–319.14. Barbera AF, Imani F, Becker T, Lezotte DC, Hobbins JC. Anatomic relationship between the pubic symphysis and ischial spines and its clinical significance in the assessment of fetal head engagement and station during labor. Ultrasound Obstet Gynecol. 2009; 33:320–325.15. Cho GJ, Hong HR, Seol HJ, Koo BH, Hong SC, Oh MJ, et al. Use of the angle of progression on ultrasonography to predict spontaneous onset of labor within 7 days. J Perinat Med. 2014; 06. 17. [Epub]. http://dx.doi.org/10.1515/jpm-2014-0106.16. Tutschek B, Braun T, Chantraine F, Henrich W. A study of progress of labour using intrapartum translabial ultrasound, assessing head station, direction, and angle of descent. BJOG. 2011; 118:62–69.17. Tutschek B, Torkildsen EA, Eggebo TM. Comparison between ultrasound parameters and clinical examination to assess fetal head station in labor. Ultrasound Obstet Gynecol. 2013; 41:425–429.18. Youssef A, Maroni E, Ragusa A, De Musso F, Salsi G, Iammarino MT, et al. Fetal head-symphysis distance: a simple and reliable ultrasound index of fetal head station in labor. Ultrasound Obstet Gynecol. 2013; 41:419–424.19. Henrich W, Dudenhausen J, Fuchs I, Kamena A, Tutschek B. Intrapartum translabial ultrasound (ITU): sonographic landmarks and correlation with successful vacuum extraction. Ultrasound Obstet Gynecol. 2006; 28:753–760.20. Ghi T, Farina A, Pedrazzi A, Rizzo N, Pelusi G, Pilu G. Diagnosis of station and rotation of the fetal head in the second stage of labor with intrapartum translabial ultrasound. Ultrasound Obstet Gynecol. 2009; 33:331–336.21. Levy R, Zaks S, Ben-Arie A, Perlman S, Hagay Z, Vaisbuch E. Can angle of progression in pregnant women before onset of labor predict mode of delivery? Ultrasound Obstet Gynecol. 2012; 40:332–337.22. Jin H, Cho G, Hong H, Seol H, Ahn K, Hong S, et al. OP07.02: Prediction of delivery mode using angle of progression, before onset of labour in nulliparous women at term. Ultrasound Obstet Gynecol. 2014; 09. 08. [Epub]. http://dx.doi.org/10.1002/uog.13696.23. Kalache KD, Duckelmann AM, Michaelis SA, Lange J, Cichon G, Dudenhausen JW. Transperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses: how well does the 'angle of progression' predict the mode of delivery? Ultrasound Obstet Gynecol. 2009; 33:326–330.24. Gilboa Y, Kivilevitch Z, Spira M, Kedem A, Katorza E, Moran O, et al. Pubic arch angle in prolonged second stage of labor: clinical significance. Ultrasound Obstet Gynecol. 2013; 41:442–446.25. Balleyguier C, Ciolovan L, Ammari S, Canale S, Sethom S, Al Rouhbane R, et al. Breast elastography: the technical process and its applications. Diagn Interv Imaging. 2013; 94:503–513.26. Hooley RJ, Scoutt LM, Philpotts LE. Breast ultrasonography: state of the art. Radiology. 2013; 268:642–659.27. Hernandez-Andrade E, Hassan SS, Ahn H, Korzeniewski SJ, Yeo L, Chaiworapongsa T, et al. Evaluation of cervical stiffness during pregnancy using semiquantitative ultrasound elastography. Ultrasound Obstet Gynecol. 2013; 41:152–161.28. Molina FS, Gomez LF, Florido J, Padilla MC, Nicolaides KH. Quantification of cervical elastography: a reproducibility study. Ultrasound Obstet Gynecol. 2012; 39:685–689.29. Hwang HS, Sohn IS, Kwon HS. Imaging analysis of cervical elastography for prediction of successful induction of labor at term. J Ultrasound Med. 2013; 32:937–946.30. Gong X, Xu Q, Xu Z, Xiong P, Yan W, Chen Y. Real-time elastography for the differentiation of benign and malignant breast lesions: a meta-analysis. Breast Cancer Res Treat. 2011; 130:11–18.31. Hee L, Sandager P, Petersen O, Uldbjerg N. Quantitative sonoelastography of the uterine cervix by interposition of a synthetic reference material. Acta Obstet Gynecol Scand. 2013; 92:1244–1249.32. Hee L, Rasmussen CK, Schlutter JM, Sandager P, Uldbjerg N. Quantitative sonoelastography of the uterine cervix prior to induction of labor as a predictor of cervical dilation time. Acta Obstet Gynecol Scand. 2014; 93:684–690.33. Feltovich H, Hall TJ, Berghella V. Beyond cervical length: emerging technologies for assessing the pregnant cervix. Am J Obstet Gynecol. 2012; 207:345–354.34. Krapp M, Baschat AA, Hankeln M, Gembruch U. Gray scale and color Doppler sonography in the third stage of labor for early detection of failed placental separation. Ultrasound Obstet Gynecol. 2000; 15:138–142.35. Herman A, Zimerman A, Arieli S, Tovbin Y, Bezer M, Bukovsky I, et al. Down-up sequential separation of the placenta. Ultrasound Obstet Gynecol. 2002; 19:278–281.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intrapartum transperineal ultrasound: angle of progression to evaluate and predict the mode of delivery and labor progression
- Neuraxial analgesia: a review of its effects on the outcome and duration of labor
- Oral Misoprostol Compared with Oral Dinoprostone for Induction of Labor at Term Pregnancy
- Vaginal Birth after Cesarean Delivery : Development of a Scoring System for Predicting Success Rate
- Transvaginal Ultrasonographic Cervical Measurement in Predicting Failed Labor Induction and Cesarean Delivery for Failure to Progress in Nulliparous Women