Korean J Urol.
2008 Jun;49(6):506-509.
Robot-assisted Laparoscopic Radical Cystectomy with Ileal Conduit Urinary Diversion
- Affiliations
-
- 1Department of Urology, Urological Science Institute and Brain Korea 21 Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea. khrha@yuhs.ac
Abstract
-
PURPOSE: In this study, we detail our initial experience with robot-assisted laparoscopic radical cystectomy(RLRC) with ileal conduit urinary diversion(ICUD) and describe the stepwise surgical procedure.
MATERIALS AND METHODS
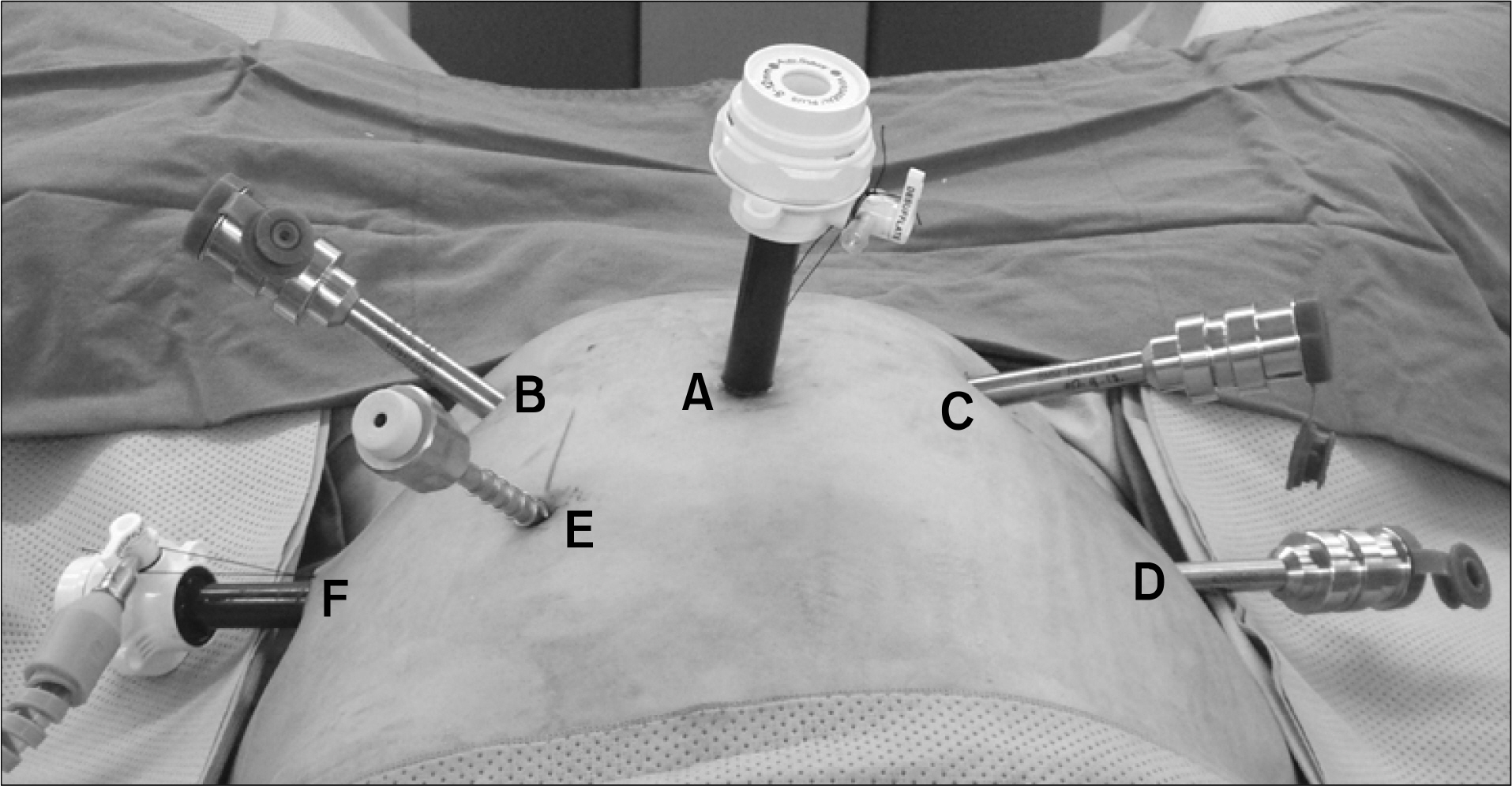
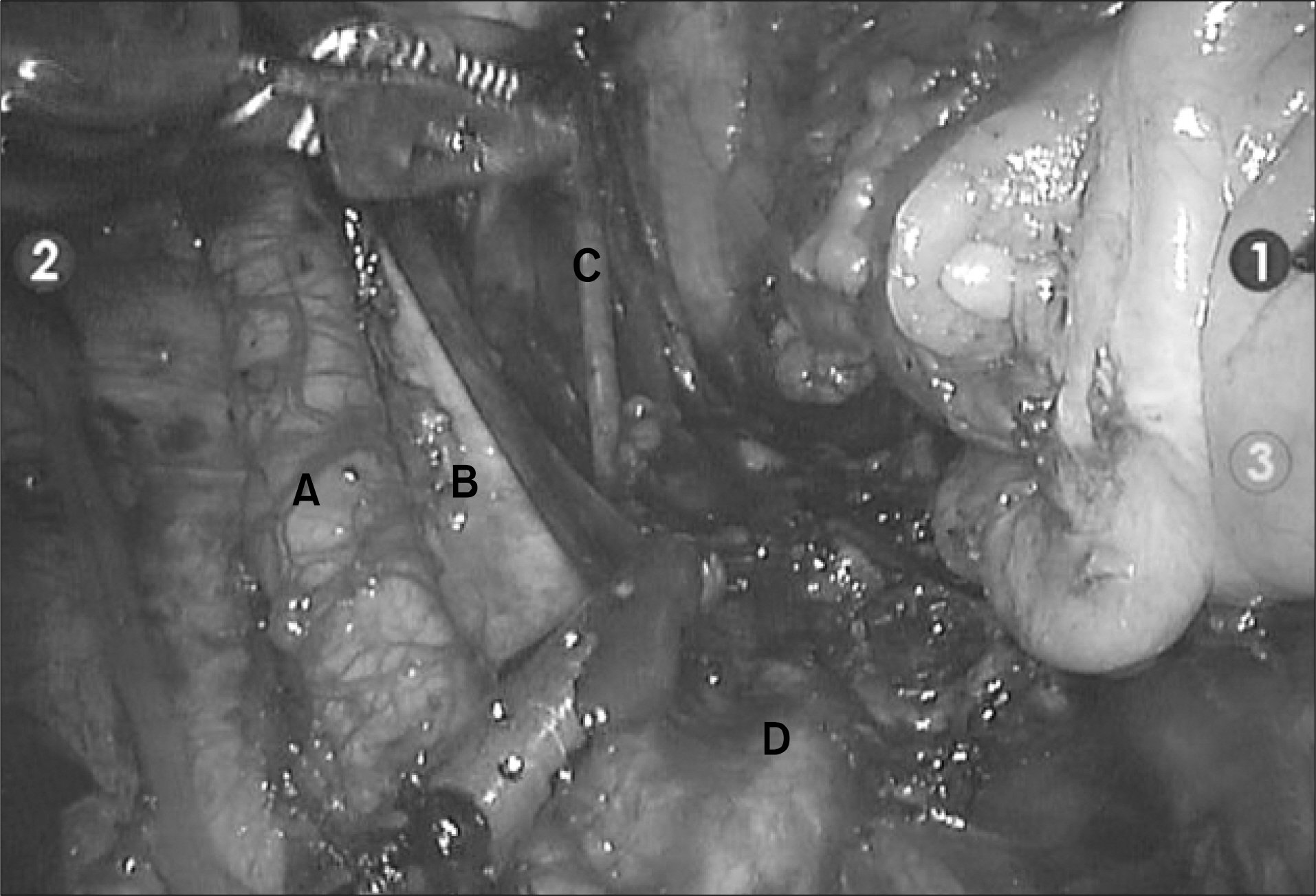
Four men underwent RLRC with extracorporeal ICUD for muscle invasive bladder cancer. RLRC was performed by a single surgeon using the da Vinci(TM) robot system(Intuitive Surgical, Sunnyvale, USA) with four robot arms. The surgical specimen was extracted through the sub-umbilical incision, and ICUD was also achieved through the sub-umbilical incision by extracorporeal technique.
RESULTS
The mean operative time was 355+/-49.8 minutes, and the mean estimated blood loss was 550+/-57.7ml. The mean hospital stay was 12+/-2.9 days. There were no major complications. On surgical pathology, one patient had pTis, one patient had pT1, and two patients had pT3 transitional cell carcinoma of the bladder. There were no positive surgical margins or lymph nodes. The mean number of dissected lymph nodes was 17+/-4.6(range: 12-23).
CONCLUSIONS
Despite limited experience, RLRC is a feasible procedure with minimal blood loss, shorter hospital stay, and may be an alternative to the open technique.
Keyword
MeSH Terms
Figure
Reference
-
1. Hemal AK, Abol-Enein H, Tewari A, Shrivastava A, Shoma AM, Ghoneim MA, et al. Robotic radical cystectomy and urinary diversion in the management of bladder cancer. Urol Clin North Am. 2004; 31:719–29.
Article2. Menon M, Hemal AK, Tewari A, Shrivastava A, Shoma AM, El-Tabey NA, et al. Nerve-sparing robot-assisted radical cystoprostatectomy and urinary diversion. BJU Int. 2003; 92:232–6.
Article3. Chang SS, Smith JA Jr, Wells N, Peterson M, Kovach B, Cookson MS. Estimated blood loss and transfusion requirements of radical cystectomy. J Urol. 2001; 166:2151–4.
Article4. Gill IS, Fergany A, Klein EA, Kaouk JH, Sung GT, Meraney AM, et al. Laparoscopic radical cystoprostatectomy with ileal conduit performed completely intracorporeally: the initial 2 cases. Urology. 2000; 56:26–9.
Article5. Gettman MT, Blute ML, Peschel R, Bartsch G. Current status of robotics in urologic laparoscopy. Eur Urol. 2003; 43:106–12.
Article6. Kwak JJ, Kim TH, Sung GT. Short term outcomes of laparoscopic radical cystectomy with an extracorporeal ileal conduit: comparative analysis with the open method. Korean J Urol. 2007; 48:938–44.
Article7. Pruthi RS, Wallen EM. Robotic-assisted laparoscopic radical cystoprostatectomy. Eur Urol. 2008; 53:310–22.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Fistula between Ileal Conduit and Iliac Artery after Radical Cystectomy with Ileal Conduit Urinary Diversion
- Robot-Assisted Laparoscopic Radical Cystectomy
- Ureteroappendicocutaneostomy(Appendix conduit): 4 Cases
- Functional Outcomes and Quality of Life after Orthotopic Bladder Substitution in Bladder Cancer Patients
- Safety of Adjuvant Chemotherapy after Orthotopic Bladder Substitution: Comparison to Ileal Conduit