Korean J Urol.
2009 Apr;50(4):355-360.
Efficacy of Ureteroscopic Removal of Stones with an Ureteral Access Sheath for the Treatment of Ureteral Calculi
- Affiliations
-
- 1Department of Urology, College of Medicine, Yeungnam University, Daegu, Korea. junghc@ynu.ac.kr
Abstract
- PURPOSE
The ureteral access sheath (UAS) was developed to facilitate difficult ureteroscopic procedures. However, some have questioned the safety of the UAS and its likelihood of causing significant ureteral traumas. We evaluated the efficacy and safety of a UAS for managing ureteral calculi. MATERIALS AND METHODS: From July 2005 to June 2008, a total of 122 patients underwent ureteroscopic removal of stones (67 patients with UAS, 55 patients without UAS). Under local, spinal, or general anesthesia, all patients were treated by using a semirigid ureteroscope with or without UAS. The operative results of the patients were assessed with KUB, and excretory urography or ultrasonography were assessed postoperatively after 2 to 4 weeks. We also analyzed the success rates of stone removal and the complication rates for each procedure. RESULTS: Mean stone size and mean operation time were 9.3 mm and 38.8 minutes, respectively, with UAS and 8.9 mm and 40.4 minutes, respectively, without UAS. Overall stone-free rates were 89.6% and 76.4%. Mean hospital stay was 2.0 days and 2.2 days. The time for operation was significantly decreased for upper ureteral stones treated with UAS (p=0.022). The stone-free rates were higher for upper ureteral stones treated with UAS (28/32, 87.5%, p=0.027), especially for stones greater than 10 mm in size (p=0.048). CONCLUSIONS: The use of UAS is effective and safe. The stone-free rates of ureteroscopic removal of stones with UAS were significantly higher than the rates without UAS for large (> or =10 mm) upper ureteral calculi.
MeSH Terms
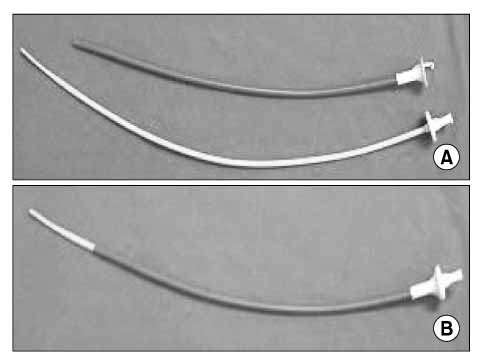
Figure
Reference
-
1. Lyon ES, Banno JJ, Schoenberg HW. Transurethral ureteroscopy in men using juvenile cystoscopy equipment. J Urol. 1979. 122:152–153.2. Netto Jr NR, Claro JF, Lemos GC, Cortade PL. Treatment options for ureteral calculi: endourology or extracorporeal schock wave lithotripsy. J Urol. 1991. 146:5–7.3. Lee YK, Park DS, Hong YK. Ureteroscopic lithotripsy with pneumatic lithotriptor: 274 cases. Korean J Urol. 2006. 47:625–630.4. Chung HS, Kim HK, Park CM. The varying success of ureteroscopic removal of stone (URS) in relation to the different locations and sizes of upper ureter stones. Korean J Urol. 2005. 46:920–924.5. Kourambas J, Byrne RR, Preminger GM. Does a ureteral access sheath facilitate ureteroscopy? J Urol. 2001. 165:789–793.6. Kim JH, Sung LH, Noh CH. Comparison between rigid ureteroscopic stone removal (URS) and extracorporeal shock wave lithotripsy (ESWL) for large (>10 mm) upper ureteral stones. Korean J Urol. 2006. 47:933–937.7. Bagley DH. Removal of upper urinary tract calculi with flexible ureteropyeloscopy. Urology. 1990. 35:412–416.8. Puppo P, Ricciotti G, Bozzo W, Introini C. Primary endoscopic treatment of ureteric calculi. A review of 378 cases. Eur Urol. 1999. 36:48–52.9. Takayasu H, Aso Y. Recent development for pyeloureteroscopy: guide tube method for its introduction into the ureter. J Urol. 1974. 112:176–178.10. Rich M, Lee WJ, Smith AD. Applications of the peel-away introducer sheath. J Urol. 1987. 137:452–454.11. Delvecchio FC, Auge BK, Brizuela RM, Weizer AZ, Silverstein AD, Lallas CD, et al. Assessment of stricture formation with the ureteral access sheath. Urology. 2003. 61:518–522.12. L'esperance JO, Ekeruo WO, Scales CD Jr, Marguet CG, Springhart WP, Maloney ME, et al. Effect of ureteral access sheath on stone-free rates in patients undergoing ureteroscopic management of renal calculi. Urology. 2005. 66:252–255.13. Pardalidis NP, Papatsoris AG, Kapotis CG, Kosmaoglou EV. Treatment of impacted lower third ureteral stones with the use of the ureteral access sheath. Urol Res. 2006. 34:211–214.14. McAleer IM, Kaplan GW, Bradley JS, Carroll SF. Staghorn calculus endotoxin expression in sepsis. Urology. 2002. 59:601.15. Rehman J, Monga M, Landman J, Lee DI, Felfela T, Conradie MC, et al. Characterization of intrapelvic pressure during ureteropyeloscopy with ureteral access sheaths. Urology. 2003. 61:713–718.16. Wu NZ, Auge BK, Preminger GM. Simplified ureteral stent placement with the assistance of a ureteral access sheath. J Urol. 2001. 166:206–208.17. Lam JS, Greene TD, Gupta M. Treatment of proximal ureteral calculi: holmium: YAG laser ureterolithotripsy versus extracorporeal shock wave lithotripsy. J Urol. 2002. 167:1972–1976.18. Chung JS, Park RJ. Ureteroscopic management of ureteral calculi: comparisons of stone basket, electrohydraulic lithotripsy, Swiss lithoclast and holmium: YAG laser. Korean J Urol. 2000. 40:239–245.19. Sofer M, Watterson JD, Wollin TA, Nott L, Razvi H, Denstedt JD. Holmium: YAG laser lithotripsy for upper urinary track calculi in 598 patients. J Urol. 2002. 167:31–34.20. Schuster TG, Hollenbeck BK, Faerber GJ, Wolf JS Jr. Complications of ureteroscopy: analysis of predictive factors. J Urol. 2001. 166:538–540.21. Abrahams HM, Stoller ML. The argument against the routine use of ureteral access sheaths. Urol Clin North Am. 2004. 31:83–87.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experience of Ureteroscopic Removal of Ureteral Stone in 35 Cases
- Experience of Ureteroscopic Removal of Stone
- Clinical Experience with Ureteroscopic Management of Ureteral Calculi Including Electrohydraulic Lithotripsy
- Ureteroscopic Manipulation of Distal Ureteral Calculi
- The Management of Ureteral Calculi with the Ureteroscopy: Failure Cases and Complications