J Korean Assoc Oral Maxillofac Surg.
2016 Jun;42(3):144-150. 10.5125/jkaoms.2016.42.3.144.
Transbuccal versus transoral approach for management of mandibular angle fractures: a prospective, clinical and radiographic study
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Hospicio District Hospital, Margao, India.
- 2Department of Oral and Maxillofacial Surgery, Goa Dental College and Hospital, Bambolim, India.
- 3Oral and Maxillofacial Surgery, Richardsons Dental and Craniofacial Hospital, Nagercoil, India. rockdotcom1386@gmail.com
- 4Department of Oral and Maxillofacial Surgery, Yogitha Dental College, Ratnagiri, India.
- 5Oral and Maxillofacial Surgery, Private Practitioner, Bengaluru, India.
- 6Department of Oral and Maxillofacial Surgery, Post Graduate Institute of Medical Sciences (PGIMS), Rohtak, India.
- KMID: 2309256
- DOI: http://doi.org/10.5125/jkaoms.2016.42.3.144
Abstract
OBJECTIVES
We compared the transbuccal and transoral approaches in the management of mandibular angle fractures.
MATERIALS AND METHODS
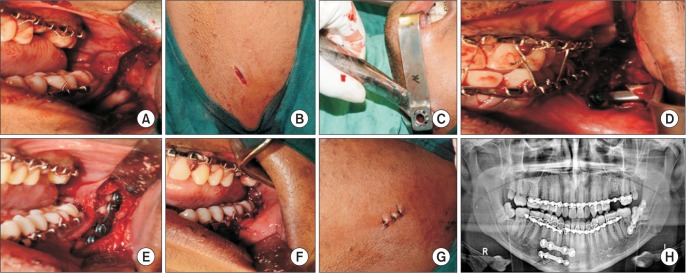
Sixty patients with mandibular angle fractures were randomly divided into two equal groups (A, transoral approach; group B, transbuccal approach) who received fracture reduction using a single 2.5 mm 4 holed miniplate with a bar using either of the two approaches. Intraoperatively, the surgical time and the ease of surgical assess for fixation were noted. Patients were followed at 1 week, 3 months, and 6 months postoperatively and evaluated clinically for post-surgical complications like scarring, infection, postoperative occlusal discrepancy, malunion, and non-union. Radiographically, the interpretation of fracture reduction was also performed by studying the fracture gap following reduction using orthopantomogram tracing. The data was tabulated and subjected to statistical analysis. A P-value less than 0.05 was considered significant.
RESULTS
No significant difference was seen between the two groups for variables like surgical time and ease of fixation. Radiographic interpretation of fracture reduction revealed statistical significance for group B from points B to D as compared to group A. No cases of malunion/non-union were noted. A single case of hypertrophic scar formation was noted in group B at 6 months postsurgery. Infection was noted in 2 patients in group B compared to 6 patients in group A. There was significantly more occlusal discrepancy in group A compared to group B at 1 week postoperatively, but no long standing discrepancy was noted in either group at the 6 months follow-up.
CONCLUSION
The transbuccal approach was superior to the transoral approach with regard to radiographic reduction of the fracture gap, inconspicuous external scarring, and fewer postoperative complications. We preferred the transbuccal approach due to ease of use, minimal requirement for plate bending, and facilitation of plate placement in the neutral mid-point area of the mandible.
MeSH Terms
Figure
Reference
-
1. Khan A, Khitab U, Khan MT, Salam A. A comparative analysis of rigid and non-rigid fixation in mandibular fractures: a prospective study. Pak Oral Dental J. 2010; 30:62–67.2. Fox AJ, Kellman RM. Mandibular angle fractures: two-miniplate fixation and complications. Arch Facial Plast Surg. 2003; 5:464–469. PMID: 14623682.3. Toma VS, Mathog RH, Toma RS, Meleca RJ. Transoral versus extraoral reduction of mandible fractures: a comparison of complication rates and other factors. Otolaryngol Head Neck Surg. 2003; 128:215–219. PMID: 12601317.
Article4. Wan K, Williamson RA, Gebauer D, Hird K. Open reduction and internal fixation of mandibular angle fractures: does the transbuccal technique produce fewer complications after treatment than the transoral technique? J Oral Maxillofac Surg. 2012; 70:2620–2628. PMID: 22959879.
Article5. Dierks EJ. Transoral approach to fractures of the mandible. Laryngoscope. 1987; 97:4–6. PMID: 3796174.
Article6. Devireddy SK, Kishore Kumar RV, Gali R, Kanubaddy SR, Dasari MR, Akheel M. Transoral versus extraoral approach for mandibular angle fractures: a comparative study. Indian J Plast Surg. 2014; 47:354–361. PMID: 25593420.
Article7. Subramanian B, Krishnamurthy S, Suresh Kumar P, Saravanan B, Padhmanabhan M. Comparison of various approaches for exposure of infraorbital rim fractures of zygoma. J Maxillofac Oral Surg. 2009; 8:99–102. PMID: 23139484.
Article8. Laverick S, Siddappa P, Wong H, Patel P, Jones DC. Intraoral external oblique ridge compared with transbuccal lateral cortical plate fixation for the treatment of fractures of the mandibular angle: prospective randomised trial. Br J Oral Maxillofac Surg. 2012; 50:344–349. PMID: 22421389.
Article9. Barry CP, Kearns GJ. Superior border plating technique in the management of isolated mandibular angle fractures: a retrospective study of 50 consecutive patients. J Oral Maxillofac Surg. 2007; 65:1544–1549. PMID: 17656281.
Article10. Sugar AW, Gibbons AJ, Patton DW, Silvester KC, Hodder SC, Gray M, et al. A randomised controlled trial comparing fixation of mandibular angle fractures with a single miniplate placed either transbuccally and intra-orally, or intra-orally alone. Int J Oral Maxillofac Surg. 2009; 38:241–245. PMID: 19167189.
Article11. Gear AJ, Apasova E, Schmitz JP, Schubert W. Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg. 2005; 63:655–663. PMID: 15883941.
Article12. Kumar GB, Dhupar V, Akkara F, Kumar SP. Patterns of maxillofacial fractures in Goa. J Maxillofac Oral Surg. 2015; 14:138–141. PMID: 26028827.
Article13. Meisami T, Sojat A, Sàndor GK, Lawrence HP, Clokie CM. Impacted third molars and risk of angle fracture. Int J Oral Maxillofac Surg. 2002; 31:140–144. PMID: 12102410.
Article14. Kroon FH, Mathisson M, Cordey JR, Rahn BA. The use of miniplates in mandibular fractures. An in vitro study. J Craniomaxillofac Surg. 1991; 19:199–204. PMID: 1894737.15. Choi BH, Kim KN, Kang HS. Clinical and in vitro evaluation of mandibular angle fracture fixation with the two-miniplate system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 79:692–695. PMID: 7621024.
Article16. Ellis E 3rd, Walker LR. Treatment of mandibular angle fractures using one noncompression miniplate. J Oral Maxillofac Surg. 1996; 54:864–871. PMID: 8676232.
Article17. Al-Moraissi EA, Ellis E 3rd. What method for management of unilateral mandibular angle fractures has the lowest rate of postoperative complications? A systematic review and meta-analysis. J Oral Maxillofac Surg. 2014; 72:2197–2211. PMID: 25236822.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The prospective preliminary clinical study of open reduction and internal fixation of mandibular angle fractures using 2 miniplates
- Treatment of Mandibular Angle Fractures
- A Study of Correlation Between Mandibular Angle Fracture and the Mandibular Third Molar
- The role of mandibular third molar in the mandibular angle fractures
- A Correlation between Mandibular Angle Fracture and the Mandibular Third Molar