Korean J Women Health Nurs.
2010 Dec;16(4):360-369. 10.4069/kjwhn.2010.16.4.360.
Development of a Sexual Health Care Scale-Practice (SHCS-P) for Oncology Nursing Care
- Affiliations
-
- 1Department of Nursing, Woosuk University, Korea. jhee90@hanmail.net
- 2College of Nursing, Nursing Policy Research Institute, Yonsei University, Korea.
- 3Department of Nursing, College of Medicine, Chung-Ang University, Korea.
- KMID: 2308197
- DOI: http://doi.org/10.4069/kjwhn.2010.16.4.360
Abstract
- PURPOSE
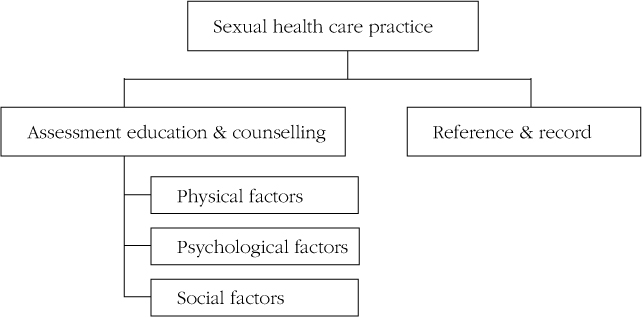
The purpose of this study was to develop and validate the Sexual Health Care Scale-Practice (SHCS-P) for oncology nurses to use in nursing care.
METHODS
Apreliminary version of the SHCS-P of 32 items was developed based on the literature and opinion of experts. A panel of eight experts reviewed the preliminary questionnaire for content validity and consolidated the instrument, which was, then, tested with data from 342 oncology nurses in Korea.
RESULTS
Exploratory factor analysis showed that the SHCS-P explained 70.49% of the total variance. The instrument revealed four factors that were named: (1) Practice for sexual function (8 items), (2) Practice for psychological factors (6 items), (3) Practice for social problems and records (4 items), and (4) Practice for reproductive care (3 items). Internal consistency was good, asassessed by the KR 20 value of 0.91. The coefficients for the sub-factors were between 0.81 and 0.93.
CONCLUSION
This scale shows validity and reliability in evaluating the practice of oncology nurses in providing sexual health care and can be used to evaluate the level of practice well as test effects of educational interventions to improve sexual health care competency.
MeSH Terms
Figure
Cited by 3 articles
-
Sexual Health Care Attitudes and Practices of Nurses Caring for Patients with Cancer
Young Hee Chae, Young Ok Song, Soon Tae Oh, Won Hee Lee, Young Mi Min, Hyang Mi Kim, Seung A Lee, Young Sin Choi
Asian Oncol Nurs. 2015;15(1):28-36. doi: 10.5388/aon.2015.15.1.28.Factors Influencing Posttraumatic Growth of Gynecologic Oncology Patients Undergoing Chemotherapy
Sun Jeong Yun, Hye Young Kim
Korean J Women Health Nurs. 2019;25(4):409-422. doi: 10.4069/kjwhn.2019.25.4.409.Nurses’ Attitude and Practice Regarding Sexual Health Care in Patients with Cancer
Yeon Son Jeong, Jeong Yun Park
Korean J Health Promot. 2022;22(2):84-92. doi: 10.15384/kjhp.2022.22.2.84.
Reference
-
1. Bruno M. Research in cancer and sexuality. Forum: cancer, body image and sexuality. The Cancer Council South Australia. 2003. Retrieved June 10, 2009. from http://www.cancersa.org.au/i-cms_file?page=1008/CancerSexualityForum1-July03Mel.pdf.2. Butler L., Banfield V. Oncology nurses' views on the provision of sexual health in cancer care. Journal of Sexual & Reproductive Medicine. 2001. 1(1):35–39.3. Clayton H., Quinn G.P., Lee J.H., King L.M., Miree C.A., Nieder M., et al. Trends in clinical practice and nurses' attitudes about fertility preservation for pediatric patients with cancer. Oncology Nursing Forum. 2008. 35(2):249–255.4. Cort E. Nurses' attitudes to sexuality in caring for cancer patients. Nursing Times. 1998. 94(42):54–56.5. Cox A., Jenkins V., Catt S., Langridge C., Fallowfield L. Information needs and experiences: an adult of UK cancer patients. European Journal of Oncology Nursing. 2006. 10(4):263–272.6. Gamel C., Hengeveld M.W., Davis B., Van der Tweel I. Factors that influence the provision of sexual health care by Dutch cancer nurses. International Journal of Nursing Studies. 1995. 32(3):301–314.7. Gamlin R. Sexuality: A challenge for nursing practice. Nursing Times. 1999. 95(7):48–50.8. Jang K.S. A study on establishment of clinical career development model of nurses. 2000. Seoul: Yonsei University of Korea;Unpublished doctoral dissertation.9. Kautz D.D., Dickey C.A., Stevens M.A. Using research to identify why nurses do not meet established sexuality nursing care standards. Journal of Nursing Quality Assurance. 1990. 4(3):69–78.10. Kim J.H. Development and evaluation of program to strengthen the performance of sexual health nursing using e-pBL. Paper presented at the meeting of Korean Society of Nursing Science. 2010a. 01. Seoul:11. Kim J.H. Factor influencing barriers to addressing patients' sexual health among clinical nurses. Journal of Korean Academy of Adult Nursing. 2010b. 22(2):113–120.12. Kim J.H., Bae K.E., Moon H., Kang H.I. The relationships among body image, depression and sexual function in postmenopausal women. Journal of Korean Academy of Adult Nursing. 2005. 17(2):239–247.13. Kim K.H., Kwon H.J., Choi M.H., Kim J.A., Kim K.S. The relationship of sexual satisfaction and daily stress in the breast cancer patients. Journal of Korean Academy of Adult Nursing. 2009. 21(5):529–537.14. King L., Quinn G.P., Vadaparampil S.T., Gwede C.K., Miree C.A., Wilson C., et al. Oncology nurses' perceptions of barriers to discussion of fertility preservation with patients with cancer. Clinical Journal of Oncology Nursing. 2008. 12(3):467–476.15. Krebs L.U. Sexual assessment in cancer care: Concept, methods, and strategies for success. Seminars in Oncology Nursing. 2008. 24(2):80–90.16. Lavin M., Hyde A. Sexuality as an aspect of nursing care for women receiving chemotherapy for breast cancer in an Irish context. European Journal of Oncology Nursing. 2006. 10(1):10–18.17. Cancer topic. National Cancer Institute. 2009. Retrieved June 10, 2009. from http://www.cancer.gov.18. Nunnally J.C., Bernstein I.H. Psychometric theory. 1994. New York: McGraw-Hill.19. Park E.Y., Yi M. Illness experience of women with breast cancer in Korea: using feminist phenomenology. Journal of Korean Academy of Adult Nursing. 2009. 21(5):504–518.20. Reynolds K.E., Magnan M.A. Nursing attitudes and beliefs toward human sexuality: collaborative research promoting evidence-based practice. Clinical Nurse Specialist. 2005. 19(5):255–229.21. Rowland J.H., Meyerowitz B.E., Crespi C.M., Leedham B., Desmond K., Belin T.R., et al. Addressing intimacy and partner communication after breast cancer: a randomized controlled group intervention. Breast Cancer Research and Treatment. 2009. 118(1):99–111.22. Simon B., Lee S.J., Partridge A.H., Runowicz C.D. Preserving fertility after cancer. CA: A Cancer Journal for Clinicians. 2005. 55(4):211–228.23. Sung T.J. Theory and practice of development and analysis of items. 2004. 2nd ed. Seoul: Hakjisa.24. Taylor B., Davis S. Using the extended PLISSIT model to address sexual healthcare needs. Nursing Standard. 2006. 21:35–40.25. Thaler-DeMers D. Intimacy issues: sexuality, fertility, and relationships. Seminars in Oncology Nursing. 2001. 17(4):255–262.26. Vadaparampil S.T., Clayton H., Quinn G.P., King L.M., Nieder M., Wilson C. Pediatric oncology nurses' attitudes related to discussing fertility preservation with pediatric cancer patients and their families. Journal of Pediatric Oncology Nursing. 2007. 24(5):255–263.27. Wilson M.E., Williams H.A. Oncology nurses' attitudes and behaviours related to sexuality of patients with cancer. Oncology Nursing Forum. 1988. 15:49–52.28. Definition of sexual health. World Health Organization. 2004. Retrieved May 15, 2010. from http://www.ho.int/reproductivehealth/gender/sexual_health.29. Yi M., Kim J.H., Park E.Y., Kim J.N., Yu E.S. Focus group study on psychosocial distress of cancer patients. Journal of Korean Academy of Adult Nursing. 2010. 22(1):19–30.30. Zippe C.D., Jhaveri F.M., Klein E.A., Kedia S., Pasqualotto F.F., Kedia A., et al. Role of viagra after radical prostatectomy. Urology. 2000. 55(2):241–245.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nurses’ Attitude and Practice Regarding Sexual Health Care in Patients with Cancer
- Sexual Health Care Attitudes and Practices of Nurses Caring for Patients with Cancer
- Comparison of Cancer Nursing Interventions Recorded in Nursing Notes with Nursing Interventions Perceived by Nurses of an Oncology Unit: Patients with Terminal Cancer
- Perceptions of Spiritual Nursing Care Nurses and Nursing Students
- The Effects of the Nursing Practice Environment and Self-leadership on Person-centered Care Provided by Oncology Nurses