Korean J Hepatobiliary Pancreat Surg.
2014 May;18(2):43-47. 10.14701/kjhbps.2014.18.2.43.
Assessment of right liver graft perfusion effectiveness between one and two-catheter infusion methods
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2305241
- DOI: http://doi.org/10.14701/kjhbps.2014.18.2.43
Abstract
- BACKGROUNDS/AIMS
Conventional graft perfusion method using one small-caliber catheter takes a relatively long time for right liver graft perfusion, thus some modification is needed. In this study, we intended to assess the effectiveness of right liver graft perfusion methods through comparison of different infusion catheters.
METHODS
The study consisted of two parts including one bench experiment to obtain data of hydraulic infusion and one clinical trial of 40 cases on graft perfusion with one- versus two-catheter infusion methods. These two graft infusion methods were compared in terms of the perfusion time and washing-out efficiency.
RESULTS
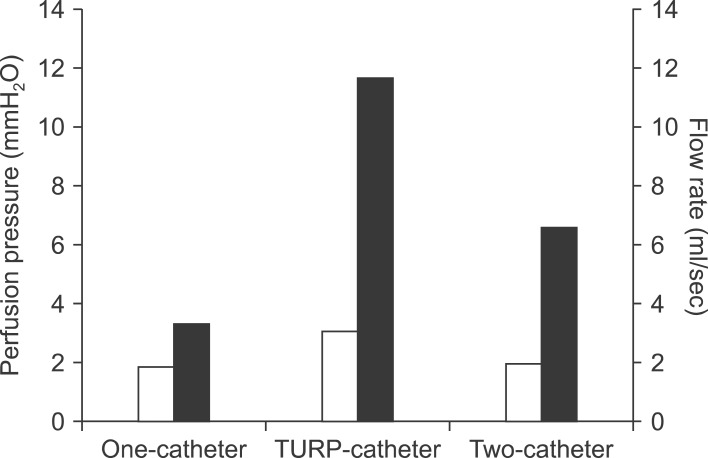
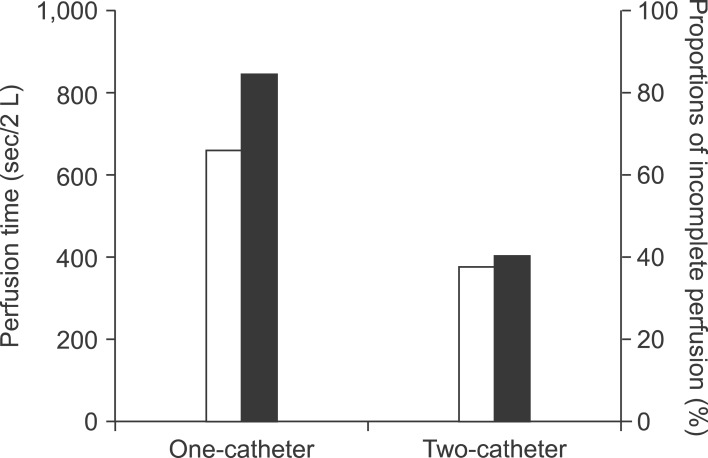
At bench experiment, the infusion flow rate and infusion pressure were 3.3 ml/sec and 1.9 cmH20 in one blood transfusion catheter group, and 11.7 ml/sec and 3.1 cmH20 in single transurethral resection of prostate irrigation catheter group, and 6.6 ml/sec and 2.0 cmH20 in two blood transfusion catheters group, respectively. In clinical trial with 40 right liver grafts, two-catheter group had a shorter graft portal perfusion time for the first 2 L of histidine-tryptophan-ketoglutarate (HTK) solution than the conventional one-catheter group (375+/-25 seconds vs. 662+/-34 seconds; p=0.001) and a lower rate of incomplete blood washing-out after the initial 2 L portal perfusion (40% vs. 85%; p=0.03).
CONCLUSIONS
The two-catheter infusion method appears to be more effective than the conventional one-catheter infusion method for right liver graft perfusion at the back table. Large size of right liver grafts seems to be its good indication.
MeSH Terms
Figure
Reference
-
1. Ozawa K, Uemoto S, Tanaka K, Kumada K, Yamaoka Y, Kobayashi N, et al. An appraisal of pediatric liver transplantation from living relatives. Initial clinical experiences in 20 pediatric liver transplantations from living relatives as donors. Ann Surg. 1992; 216:547–553. PMID: 1280074.
Article2. Hwang S, Lee SG, Kim KH, Park KM, Ahn CS, Moon DB, et al. Correlation of blood-free graft weight and volumetric graft volume by an analysis of blood content in living donor liver grafts. Transplant Proc. 2002; 34:3293–3294. PMID: 12493450.
Article3. Testa G, Malagó M, Nadalin S, Treptow B, Paul A, Frilling A, et al. Histidine-tryptophan-ketoglutarate versus University of Wisconsin solution in living donor liver transplantation: results of a prospective study. Liver Transpl. 2003; 9:822–826. PMID: 12884194.
Article4. Sato Y, Watanabe H, Ichida T, Yamamoto S, Nakatsuka H, Oya H, et al. Wall shear stress and intrahepatic leukocytes of graft in living related donor liver transplantation. Hepatogastroenterology. 2004; 51:329–333. PMID: 15086151.5. Hajeer AH, Issa S, Alaskar A, Abdullah K, Awad M, Tbakhi A, et al. Neutrophils and lymphoid chimerism after adult living-related liver transplantation from a homozygous donor. Transplant Proc. 2005; 37:4386–4388. PMID: 16387127.
Article6. Soejima Y, Shimada M, Suehiro T, Hiroshige S, Gondo H, Takami A, et al. Graft-versus-host disease following living donor liver transplantation. Liver Transpl. 2004; 10:460–464. PMID: 15004778.
Article7. Man K, Fan ST, Lo CM, Liu CL, Fung PC, Liang TB, et al. Graft injury in relation to graft size in right lobe live donor liver transplantation: a study of hepatic sinusoidal injury in correlation with portal hemodynamics and intragraft gene expression. Ann Surg. 2003; 237:256–264. PMID: 12560784.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Partial Portal Arterialization on Graft Survival in Experimental Liver Transplantation
- Liver Procurement
- Liver graft from donation after circulatory death donor: Real practice to improve graft viability
- Living-Donor Liver Transplantation with Renoportal Anastomosis using an Interposition Polytetrafluoroethylene Graft for a Patient with Large Spontaneous Splenorenal Shunt: A Case Report
- Liver abscess developed after cadaveric liver transplantation due to ligation of an accessory right hepatic artery of the donor graft