Korean Circ J.
2012 Jan;42(1):33-39. 10.4070/kcj.2012.42.1.33.
Fibro-Fatty Component is Important for the Long-Term Clinical Events in Patients Who Have Undergone Primary Percutaneous Coronary Intervention
- Affiliations
-
- 1Division of Cardiology, Konyang University College of Medicine, Daejeon, Korea. janghobae@yahoo.co.kr
- KMID: 2297905
- DOI: http://doi.org/10.4070/kcj.2012.42.1.33
Abstract
- BACKGROUND AND OBJECTIVES
We evaluated which plaque components are associated with long-term clinical events in patients who underwent primary percutaneous coronary intervention (PCI).
SUBJECTS AND METHODS
The study subjects consisted of 57 consecutive patients (mean age, 58.5+/-14.5 years; 45 males) who underwent primary PCI and a virtual histology-intravascular ultrasound examination. Major adverse cardiac events (MACEs) including death, acute myocardial infarction, stroke, and revascularization were evaluated during the mean 28 month follow-up period.
RESULTS
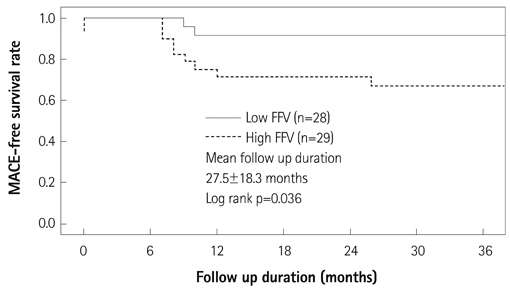
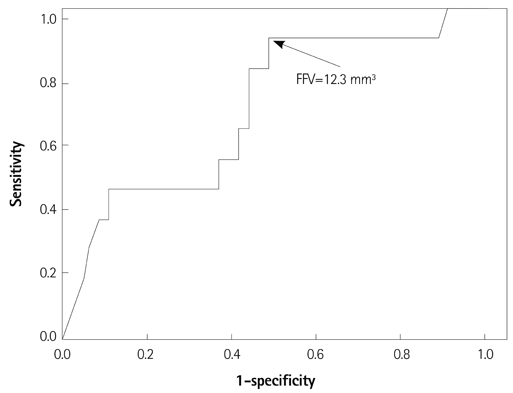
Patients with high fibro-fatty volume (FFV >13.4 mm3, n=29; mean age, 61.3 years) had a lower ejection fraction (52.7% vs. 59.4%, p=0.022), a higher incidence of multi-vessel disease (69.0% vs. 28.6%, p=0.002), larger plaque area (25.7 mm2 vs. 15.9 mm2, p<0.001), and larger plaque volume (315 mm3 vs. 142 mm3, p<0.001) than those with a low FFV (< or =13.4 mm3, n=28; mean age, 55.6 years). Patients with high FFV had a significantly higher incidence (32.1% vs. 8.3%, p=0.036) of MACE than those with low FFV. When we divided the study population according to the necrotic core volume (NCV), fibrous volume, or dense calcified volume, no significant findings in terms of demographics and MACE rates were observed. A Cox regression analysis revealed that the independent factor for MACE was FFV (hazard ratio, 6.748; 95% confidence interval, 1.168-38.971, p=0.033) in this study population.
CONCLUSION
The coronary plaque component, particularly FFV, but not NCV, was important in long-term clinical outcomes in patients who underwent primary PCI.
MeSH Terms
Figure
Reference
-
1. Nair A, Kuban BD, Tuzcu EM, et al. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002. 106:2200–2206.2. Virmani R, Burke AP, Kolodgie FD, Farb A. Vulnerable plaque: the pathology of unstable coronary lesions. J Interv Cardiol. 2002. 15:439–446.3. Rodriguez-Granillo GA, McFadden EP, Valgimigli M, et al. Coronary plaque composition of nonculprit lesions, assessed by in vivo intracoronary ultrasound radio frequency data analysis, is related to clinical presentation. Am Heart J. 2006. 151:1020–1024.4. Böse D, von Birgelen C, Zhou XY, et al. Impact of atherosclerotic plaque composition on coronary microembolization during percutaneous coronary interventions. Basic Res Cardiol. 2008. 103:587–597.5. Kawaguchi R, Oshima S, Jingu M, et al. Usefulness of virtual histology intravascular ultrasound to predict distal embolization for ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2007. 50:1641–1646.6. Missel E, Mintz GS, Carlier SG, et al. Necrotic core and its ratio to dense calcium are predictors of high-risk non-ST-elevation acute coronary syndrome. Am J Cardiol. 2008. 101:573–578.7. Hong MK, Mintz GS, Lee CW, et al. Comparison of virtual histology to intravascular ultrasound of culprit coronary lesions in acute coronary syndrome and target coronary lesions in stable angina pectoris. Am J Cardiol. 2007. 100:953–959.8. Rodriguez-Granillo GA, Serruys PW, Garcia-Garcia HM, et al. Coronary artery remodelling is related to plaque composition. Heart. 2006. 92:388–391.9. Kataoka T, Mathew V, Rubinshtein R, et al. Association of plaque composition and vessel remodeling in atherosclerotic renal artery stenosis: a comparison with coronary artery disease. JACC Cardiovasc Imaging. 2009. 2:327–338.10. Fujii K, Carlier SG, Mintz GS, et al. Association of plaque characterization by intravascular ultrasound virtual histology and arterial remodeling. Am J Cardiol. 2005. 96:1476–1483.11. Surmely JF, Nasu K, Fujita H, et al. Association of coronary plaque composition and arterial remodelling: a virtual histology analysis by intravascular ultrasound. Heart. 2007. 93:928–932.12. Bae JH, Kwon TG, Hyun DW, Rihal CS, Lerman A. Predictors of slow flow during primary percutaneous coronary intervention: an intravascular ultrasound-virtual histology study. Heart. 2008. 94:1559–1564.13. Nakamura T, Kubo N, Ako J, Momomura S. Angiographic no-reflow phenomenon and plaque characteristics by virtual histology intravascular ultrasound in patients with acute myocardial infarction. J Interv Cardiol. 2007. 20:335–339.14. Higashikuni Y, Tanabe K, Tanimoto S, et al. Impact of culprit plaque composition on the no-reflow phenomenon in patients with acute coronary syndrome: an intravascular ultrasound radiofrequency analysis. Circ J. 2008. 72:1235–1241.15. Hong YJ, Jeong MH, Choi YH, et al. Impact of plaque components on no-reflow phenomenon after stent deployment in patients with acute coronary syndrome: a virtual histology-intravascular ultrasound analysis. Eur Heart J. 2009. doi: 10.1093/eurheartj/ehp034.16. Tobis JM, Mallery J, Mahon D, et al. Intravascular ultrasound imaging of human coronary arteries in vivo: analysis of tissue characterizations with comparison to in vitro histological specimens. Circulation. 1991. 83:913–926.17. Mintz GS, Nissen SE, Anderson WD, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascluar Ultrasound Studies (IVUS): a report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001. 37:1478–1492.18. Resnic FS, Wainstein M, Lee MK, et al. No-reflow is an independent predictor of death and myocardial infarction after percutaneous coronary intervention. Am Heart J. 2003. 145:42–46.19. Ramírez-Moreno A, Cardenal R, Pera C, et al. Predictors and prognostic value of myocardial injury following stent implantation. Int J Cardiol. 2004. 97:193–198.20. Yip HK, Chen MC, Chang HW, et al. Angiographic morphologic features of infarct-related arteries and timely reperfusion in acute myocardial infarction: predictors of slow-flow and no-reflow phenomenon. Chest. 2002. 122:1322–1332.21. Kawamoto T, Okura H, Koyama Y, et al. The relationship between coronary plaque characteristics and small embolic particles during coronary stent implantation. J Am Coll Cardiol. 2007. 50:1635–1640.22. Henriques de Gouveia R, van der Wal AC, van der Loos CM, Becker AE. Sudden unexpected death in young adults: discrepancies between initiation of acute plaque complications and the onset of acute coronary death. Eur Heart J. 2002. 23:1433–1440.23. Murakami T, Mizuno S, Takahashi Y, et al. Intracoronary aspiration thrombectomy for acute myocardial infarction. Am J Cardiol. 1998. 82:839–844.24. Nasu K, Tsuchikane E, Katoh O, et al. Accuracy of in vivo coronary plaque morphology assessment: a validation study of in vivo virtual histology compared with in vitro histopathology. J Am Coll Cardiol. 2006. 47:2405–2412.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treat or Not to Treat Non-culprit Coronary Artery with Significant Stenosis during Primary Percutaneous Coronary Intervention
- Recent Advances in Percutaneous Coronary Intervention in Coronary Artery Disease
- Cardiac CT in Detecting a Dislodged Stent in Right Coronary Artery after Primary Percutaneous Coronary Intervention
- De-escalation strategies of dual antiplatelet therapy in patients undergoing percutaneous coronary intervention for acute coronary syndrome
- Long-term Clinical and Angiographic Results of Coronary Stenting in Diabetic Patients