Korean J Urol.
2006 Jun;47(6):645-650. 10.4111/kju.2006.47.6.645.
Therapeutic Efficacy of Extracorporeal Magnetic Therapy on Low Urinary Tract Symptoms and Sexual Function in Chronic Pelvic Pain Syndrome
- Affiliations
-
- 1Department of Urology, Sung Ae General Hospital, Seoul, Korea. urokhj@dreamwiz.com
- KMID: 2294241
- DOI: http://doi.org/10.4111/kju.2006.47.6.645
Abstract
-
PURPOSE: To find whether extracorporeal magnetic innervation (ExMi) changes the low urinary tract symptoms and sexual function in patients with chronic pelvic pain syndrome (CPPS).
MATERIALS AND METHODS
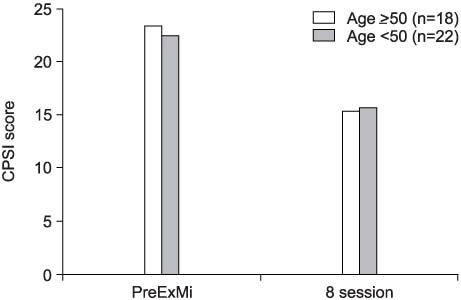
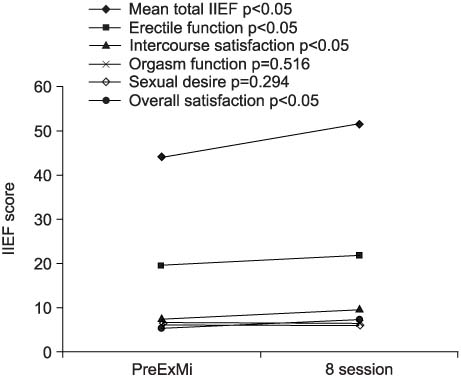
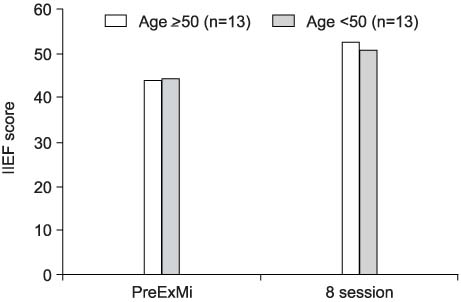
ExMi treatment was performed in 51 patients, diagnosed as National Institute of Health (NIH) type III prostatitis, with each treatment session composed of 10 min at 40Hz, 2 min rest and 10 min at 50Hz. Both before and after the completion of 8 sessions of ExMi, self-administered NIH-chronic prostatitis symptom index (NIH-CPSI) and International Index of Erectile Function (IIEF) questionnaires were completed to assess the changes in the patient's symptoms.
RESULTS
Following the ExMi treatment, 25 of the 40 patients experienced a 30% or greater improvement of low urinary tract symptoms. The total NIH-CPSI scores ranged from 22.4 to 15.6 (p<0.05). Each domain of the NIH-CPSI was as follows: pain, from 9.0 to 6.2; urination, from 6.7 to 4.8 and effect on the quality of life, from 6.6 to 4.5, and 11 of the 26 patients experienced a 15% or greater improvement of their sexual function. The mean total IIEF scores ranged from 44.1+/-13.5 to 51.6+/-11.3 (p<0.05). Each domain of the IIEF was as follows: erectile function, from 19.5 7.0 to 21.7+/-5.6 (p<0.05); intercourse satisfaction, from 7.4+/-2.2 to 9.5+/-2.2 (p<0.05); orgasm function, from 6.5+/-2.2 to 6.6+/-2.6 (p=0.516); sexual desire, from 6.2+/-1.9 to 6.3+/-1.6 (p=0.294) and overall satisfaction from 5.4+/-1.5 to 7.3+/-1.3 (p<0.05).
CONCLUSIONS
result, ExMi was shown to reduce the lower urinary tract symptoms, and enhances the sexual function in CPPS, suggesting ExMi is effective and may help in the management of CPPS.
Keyword
MeSH Terms
Figure
Reference
-
1. Collins MM, Stafford RS, O'Leary P, Barry MJ. How common is prostatitis? A national survey of physician visits. J Urol. 1997. 157:Suppl. 243A. abstract 950.2. Wenninger K, Heiman JR, Rothman I, Berghuis JP, Berger RE. Sickness impact of chronic nonbacterial prostatitis and its correlates. J Urol. 1996. 155:965–968.3. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236–237.4. Nickel JC, Nyberg LM, Hennenfent M. Research guidelines for chronic prostatitis: consensus report from the first National Institutes of Health International Prostatitis Collaborative Network. Urology. 1999. 54:229–233.5. Lee KS, Yoon JM, Cho IR. NIH-chronic prostatitis symptom index (NIH-CPSI). Prostate update 5 year. 2002. 1:108–121.6. Oh SH, Oh BR, Ryu SB. Effect of finasteride on sexual function in patients with benign prostatic hyperplasia. Korean J Urol. 2002. 43:611–618.7. Brahler E. Weidner W, Madsen PO, Schiefer HG, editors. Complaint complexes and psychosomatic aspects. Prostatitis etipathology, diagnosis and treatment. 1994. 1st ed. Berlin: Springer-Verlag;40–48.8. Krieger JN, Egan KJ, Ross SO, Jacobs R, Berger RE. Chronic pelvic pains represent the most prominant urogenital symptoms of "chronic prostatitis". Urology. 1996. 48:715–722.9. Cho IR, Park SC, Park SS. The prevalence of the symptoms of the prostate syndrome patients under 50. Korean J Urol. 1998. 39:751–756.10. Krieger JN, Ross SO, Riley DE. Chronic prostatitis; epidemiology and role of infection. Urology. 2002. 60:6 Suppl. 8–12.11. Pontari MA, Ruggieri MR. Mechanisms in prostatitis/chronic pelvic pain syndrome. J Urol. 2004. 172:839–845.12. El-Hakim A, Shah DK, Smith AD. Advanced therapy for prostatitis: minimally invasive and invasive therapies. Curr Urol Rep. 2003. 4:320–326.13. Zvara P, Folsom JB, Plante MK. Minimally invasive therapies for prostatitis. Curr Urol Rep. 2004. 5:320–326.14. Yamanishi T, Yasuda K, Suda S, Ishikawa N. Effect of functional continuous magnetic stimulation on urethral closure in healthy volunteers. Urology. 1999. 54:652–655.15. Hallett M, Cohen LG. Magnetism. A new method for stimulation of nerve and brain. JAMA. 1989. 262:538–541.16. Roth BJ, Cohen LG, Hallett M. The electric field induced during magnetic stimulation. Electroencephalogr Clin Neurophysiol. 1991. 43:Suppl. 268–278.17. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965. 150:971–979.18. Guskov AR, Vasiliev AI. An electrostimulator to restore sexual function in chronic prostatitis patients. Med Prog Technol. 1992. 18:43–46.19. Kim SW, Kim SH, Lee CH, Lee SJ, Cho YH, Yoon MS. Clinical efficacy of extracorporeal magnetic innervation for chronic pelvic pain syndrome. Korean J Androl. 2003. 21:44–47.20. Lee KC, Choi H, Park HS, Kim JJ, Moon DG. Therapeutic efficacy of extracorporeal magnetic therapy in chronic pelvic pain syndrome. Korean J Urol. 2003. 44:693–696.21. Leippold T, Strebel RT, Huwyler M, John HA, Hauri D, Schmid DM. Sacral magnetic stimulation in non-inflammatory chronic pelvic pain syndrome. BJU Int. 2005. 95:838–841.22. Galloway NT, El-Galley RE, Sand PK, Appell RA, Russell HW, Carlan SJ. Extracorporeal magnetic innervation therapy for stress urinary incontinence. Urology. 1999. 53:1108–1111.23. Kim KH, Hong JY, Yoon HN. Early experience with extracorporeal magnetic innervation (ExMI) therapy for stress urinary incontinence. Korean J Urol. 2001. 42:938–941.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Therapeutic Efficacy of Extracorporeal Magnetic Therapy in Chronic Pelvic Pain Syndrome
- Is Urethral Pain Syndrome Really Part of Bladder Pain Syndrome?
- The Effect of Extracorporeal Magnetic Innervation Therapy on Pain, Urination and Quality of Life in Chronic Pelvic Pain Syndrome
- A Study on the Improvement of Urinary Incontinence Symptoms and Sexual Function in Patients with Urinary Incontinence before and after Extracorporeal Magnetic Innervation (ExMI) Therapy
- UPOINT System: A Diagnostic/Therapeutic Algorithm for Chronic Prostatitis/Chronic Pelvic Pain Syndrome