Ann Surg Treat Res.
2014 Mar;86(3):115-121. 10.4174/astr.2014.86.3.115.
The pattern and significance of the calcifications of papillary thyroid microcarcinoma presented in preoperative neck ultrasonography
- Affiliations
-
- 1Department of Thyroid and Endocrine Surgery, Gachon University Gil Medical Center, Incheon, Korea. peacemk@gilhospital.com
- KMID: 2266891
- DOI: http://doi.org/10.4174/astr.2014.86.3.115
Abstract
- PURPOSE
To analyze the incidence and patterns of calcification of papillary thyroid microcarcinoma (PTMC) on neck ultrasonography (NUS) and assess the clinical implications of calcification, especially for neck node metastasis.
METHODS
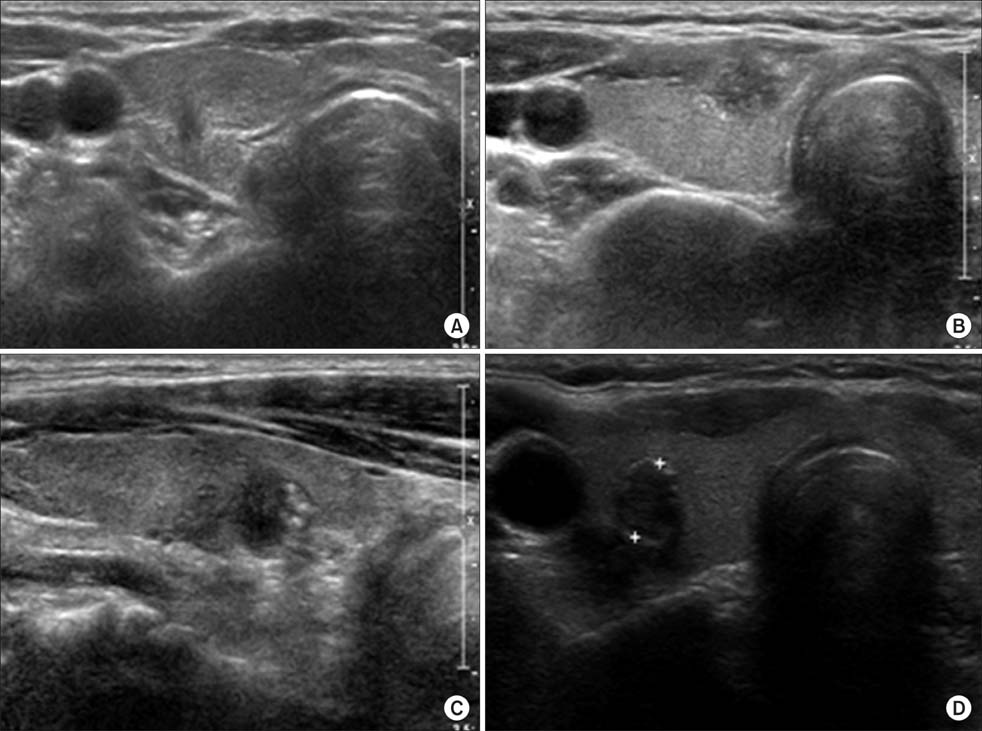
The clinical data of 379 patients with PTMC who underwent thyroidectomy between January and December 2011 were retrospectively analyzed. PTMC lesions were classified into four subgroups according to their calcification patterns on preoperative NUS: microcalcification, macrocalcification, rim calcification, and noncalcification. The clinicopathologic characteristics were compared between the patients with and without calcification, and among the four subgroups.
RESULTS
Calcifications were detected on NUS in 203 patients (53.5%) and central neck node metastasis was observed in 119 patients (31.3%). Calcification was associated with larger tumor size (0.68 cm vs. 0.54 cm), higher rate of lymph node metastasis (38.6% vs. 23.2%) and higher lymph node ratio (0.11 vs. 0.06) compared to noncalcification (All P < 0.05). In addition, the extent of calcification correlated with lesion size (0.67 cm vs. 0.69 cm vs. 0.85 cm). Further, the likelihood of lymph node metastasis also correlated with the extent of calcification in the order of non-, micro- and macrocalcification (23.3%, 36.8%, and 44.1%, respectively). The calcification rate was higher in patients with lymph node metastasis than those without it (65.5% vs.47.7%) (All P < 0.05).
CONCLUSION
PTMC patients positive for calcification on NUS had a higher rate of lymph node metastasis, and a higher lymph node ratio compared to noncalcification patients. Calcification patterns should be assessed carefully in patients with PTMC by preoperative NUS.
MeSH Terms
Figure
Reference
-
1. Ito Y, Uruno T, Nakano K, Takamura Y, Miya A, Kobayashi K, et al. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid. 2003; 13:381–387.2. Koike E, Noguchi S, Yamashita H, Murakami T, Ohshima A, Kawamoto H, et al. Ultrasonographic characteristics of thyroid nodules: prediction of malignancy. Arch Surg. 2001; 136:334–337.3. Khoo ML, Asa SL, Witterick IJ, Freeman JL. Thyroid calcification and its association with thyroid carcinoma. Head Neck. 2002; 24:651–655.4. Takashima S, Fukuda H, Nomura N, Kishimoto H, Kim T, Kobayashi T. Thyroid nodules: re-evaluation with ultrasound. J Clin Ultrasound. 1995; 23:179–184.5. Seiberling KA, Dutra JC, Grant T, Bajramovic S. Role of intrathyroidal calcifications detected on ultrasound as a marker of malignancy. Laryngoscope. 2004; 114:1753–1757.6. Johannessen JV, Sobrinho-Simoes M. The origin and significance of thyroid psammoma bodies. Lab Invest. 1980; 43:287–296.7. Das DK, Sheikh ZA, George SS, Al-Baquer T, Francis IM. Papillary thyroid carcinoma: evidence for intracytoplasmic formation of precursor substance for calcification and its release from well-preserved neoplastic cells. Diagn Cytopathol. 2008; 36:809–812.8. Tunio GM, Hirota S, Nomura S, Kitamura Y. Possible relation of osteopontin to development of psammoma bodies in human papillary thyroid cancer. Arch Pathol Lab Med. 1998; 122:1087–1090.9. Sun Y, Fang S, Dong H, Zhao C, Yang Z, Li P, et al. Correlation between osteopontin messenger RNA expression and microcalcification shown on sonography in papillary thyroid carcinoma. J Ultrasound Med. 2011; 30:765–771.10. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, et al. Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology. 2008; 247:762–770.11. Frates MC, Benson CB, Charboneau JW, Cibas ES, Clark OH, Coleman BG, et al. Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology. 2005; 237:794–800.12. Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002; 87:1941–1946.13. Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002; 178:687–691.14. Wang N, Xu Y, Ge C, Guo R, Guo K. Association of sonographically detected calcification with thyroid carcinoma. Head Neck. 2006; 28:1077–1083.15. Wang Y, Li L, Wang YX, Feng XL, Zhao F, Zou SM, et al. Ultrasound findings of papillary thyroid microcarcinoma: a review of 113 consecutive cases with histopathologic correlation. Ultrasound Med Biol. 2012; 38:1681–1688.16. Kuma K, Matsuzuka F, Kobayashi A, Hirai K, Morita S, Miyauchi A, et al. Outcome of long standing solitary thyroid nodules. World J Surg. 1992; 16:583–587.17. Kwak MS, Baek JH, Kim YS, Jeong HJ. Patterns and significance of peripheral calcifications of thyroid tumors seen on ultrasound. J Korean Radiol Soc. 2005; 53:401–405.18. Bai Y, Zhou G, Nakamura M, Ozaki T, Mori I, Taniguchi E, et al. Survival impact of psammoma body, stromal calcification, and bone formation in papillary thyroid carcinoma. Mod Pathol. 2009; 22:887–894.19. Triggiani V, Guastamacchia E, Licchelli B, Tafaro E. Microcalcifications and psammoma bodies in thyroid tumors. Thyroid. 2008; 18:1017–1018.20. Ellison E, Lapuerta P, Martin SE. Psammoma bodies in fine-needle aspirates of the thyroid: predictive value for papillary carcinoma. Cancer. 1998; 84:169–175.21. Klinck GH, Winship T. Psammoma bodies and thyroid cancer. Cancer. 1959; 12:656–662.22. Hopkins DR, Keles S, Greenspan DS. The bone morphogenetic protein 1/Tolloid-like metalloproteinases. Matrix Biol. 2007; 26:508–523.23. Senger DR, Wirth DF, Hynes RO. Transformed mammalian cells secrete specific proteins and phosphoproteins. Cell. 1979; 16:885–893.24. Oldberg A, Franzen A, Heinegard D. Cloning and sequence analysis of rat bone sialoprotein (osteopontin) cDNA reveals an Arg-Gly-Asp cell-binding sequence. Proc Natl Acad Sci U S A. 1986; 83:8819–8823.25. Sharp JA, Sung V, Slavin J, Thompson EW, Henderson MA. Tumor cells are the source of osteopontin and bone sialoprotein expression in human breast cancer. Lab Invest. 1999; 79:869–877.26. Hirota S, Ito A, Nagoshi J, Takeda M, Kurata A, Takatsuka Y, et al. Expression of bone matrix protein messenger ribonucleic acids in human breast cancers. Possible involvement of osteopontin in development of calcifying foci. Lab Invest. 1995; 72:64–69.27. Bellahcène A, Castronovo V. Expression of bone matrix proteins in human breast cancer: potential roles in microcalcification formation and in the genesis of bone metastases. Bull Cancer. 1997; 84:17–24.28. Guarino V, Faviana P, Salvatore G, Castellone MD, Cirafici AM, De Falco V, et al. Osteopontin is overexpressed in human papillary thyroid carcinomas and enhances thyroid carcinoma cell invasiveness. J Clin Endocrinol Metab. 2005; 90:5270–5278.29. Carcangiu ML, Zampi G, Pupi A, Castagnoli A, Rosai J. Papillary carcinoma of the thyroid. A clinicopathologic study of 241 cases treated at the University of Florence, Italy. Cancer. 1985; 55:805–828.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ectopic Thyroid Papillary Carcinoma with Incidental Papillary Thyroid Microcarcinoma
- Annual Neck Ultrasonography Surveillance between 3 to 12 Years after Thyroid Lobectomy for Papillary Thyroid Microcarcinoma
- Ultrasonographic Findings of Papillary Thyroid Cancer with or without Hashimoto's Thyroiditis
- Papillary Thyroglossal Duct Cyst Carcinoma with Synchronous Occult Papillary Thyroid Microcarcinoma
- A Case of Cystic Lymph Node Metastasis from Thyroid Papillary Microcarcinoma