Ann Surg Treat Res.
2015 Mar;88(3):126-132. 10.4174/astr.2015.88.3.126.
Early outcome of the Korean Diagnosis-Related Groups payment system for appendectomy
- Affiliations
-
- 1Department of Surgery, Seoul Metropolitan Government - Seoul National University Boramae Medical Center, Seoul, Korea. imjung@brm.co.kr
- KMID: 2266869
- DOI: http://doi.org/10.4174/astr.2015.88.3.126
Abstract
- PURPOSE
The implementation of the Korean diagnosis-related groups (DRG) payment system has been recently introduced in selected several diseases including appendectomy in Korea. Here, we report the early outcomes with regard to clinical aspects and medical costs of the Korean DRG system for appendectomies in Seoul Metropolitan Government - Seoul National University Boramae Medical Center throughout comparing before and after introduction of DRG system.
METHODS
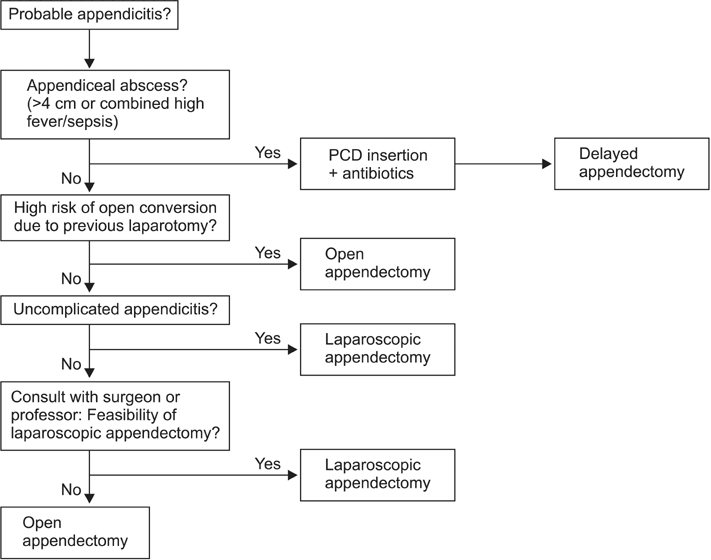
The DRG system was applied since January 2013 at our institute. After the DRG system, we strategically designed and applied our algorithm for the treatment of probable appendicitis. We reviewed the patients who were treated with a procedure of appendectomy for probable appendicitis between July 2012 and June 2013, divided two groups based on before and after the application of DRG system, and compared clinical outcomes and medical costs.
RESULTS
Total 416 patients were included (204 patients vs. 212 patients in the group before vs. after DRG). Shorter hospital stays (2.98 +/- 1.77 days vs. 3.82 +/- 1.84 days, P < 0.001) were found in the group after DRG. Otherwise, there were no significant differences in the perioperative outcomes and medical costs including costs for first hospitalization and operation, costs for follow-up after discharge, frequency of visits of out-patient's clinic or Emergency Department or rehospitalization.
CONCLUSION
In the Korean DRG system for appendectomy, there were no significant differences in perioperative outcomes and medical costs, except shorter hospital stay. Further studies should be continued to evaluate the current Korean DRG system for appendectomy and further modifications and supplementations are needed in the future.
MeSH Terms
Figure
Reference
-
1. Fourie C, Biller-Andorno N, Wild V. Systematically evaluating the impact of diagnosis-related groups (DRGs) on health care delivery: a matrix of ethical implications. Health Policy. 2014; 115:157–164.2. Mathauer I, Wittenbecher F. Hospital payment systems based on diagnosis-related groups: experiences in low- and middleincome countries. Bull World Health Organ. 2013; 91:746A–756A.3. Yoo RN, Chung CW, Kim JW. Evaluating the efficacy of the current diagnosis-related group reimbursement system for laparoscopic appendectomy at a single institute in Korea. Ann Surg Treat Res. 2014; 87:148–155.4. Geissler A, Scheller-Kreinsen D, Quentin W. EuroDRG group. Do diagnosis-related groups appropriately explain variations in costs and length of stay of hip replacement? A comparative assessment of DRG systems across 10 European countries. Health Econ. 2012; 21:Suppl 2. 103–115.5. Ellis RP. Creaming, skimping and dumping: provider competition on the intensive and extensive margins. J Health Econ. 1998; 17:537–555.6. Martinussen PE, Hagen TP. Reimbursement systems, organisational forms and patient selection: evidence from day surgery in Norway. Health Econ Policy Law. 2009; 4(Pt 2):139–158.7. Lee JH, Park YS, Choi JS. The epidemiology of appendicitis and appendectomy in South Korea: national registry data. J Epidemiol. 2010; 20:97–105.8. Quentin W, Scheller-Kreinsen D, Geissler A, Busse R. EuroDRG group. Appendectomy and diagnosis-related groups (DRGs): patient classification and hospital reimbursement in 11 European countries. Langenbecks Arch Surg. 2012; 397:317–326.9. Mason A, Or Z, Renaud T, Street A, Thuilliez J, Ward P, et al. How well do diagnosis-related groups for appendectomy explain variations in resource use? An analysis of patient-level data from 10 European countries. Health Econ. 2012; 21:Suppl 2. 30–40.10. Street A, Sivey P, Mason A, Miraldo M, Siciliani L. Are English treatment centres treating less complex patients? Health Policy. 2010; 94:150–157.11. Yuk JS, Kim YJ, Hur JY, Shin JH. Association between pregnancy and acute appendicitis in South Korea: a population-based, cross-sectional study. J Korean Surg Soc. 2013; 85:75–79.12. Schreyogg J. A micro-costing approach to estimating hospital costs for appendectomy in a cross-European context. Health Econ. 2008; 17:1 Suppl. S59–S69.13. Williams MD, Collins JN, Wright TF, Fenoglio ME. Laparoscopic versus open appendectomy. South Med J. 1996; 89:668–674.14. Yau KK, Siu WT, Tang CN, Yang GP, Li MK. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg. 2007; 205:60–65.15. Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S, et al. Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg. 2004; 239:43–52.16. Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2010; (10):CD001546.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Case-Payment System in Vascular Surgery
- Changes in the Mixed Fee-Based Payment System in Primary Care: Cases and Implications
- Current Status and Future Directions of Primary Care in the World: Insights from United States (1) —Primary Care and Payment Reform—
- Forecasting the Future Reimbursement System of Korean National Health Insurance: A Contemplation Focusing on Global Budget and Neo-KDRG-Based Payment Systems
- Participation Determinants in the DRG Payment System of Obstetrics and Gynecology Clinics in South Korea