Ann Rehabil Med.
2012 Feb;36(1):126-132. 10.5535/arm.2012.36.1.126.
The Significance of Transcutaneous Continuous Overnight CO2 Monitoring in Determining Initial Mechanical Ventilator Application for Patients with Neuromuscular Disease
- Affiliations
-
- 1Department of Rehabilitation Medicine and Rehabilitation Institute of Muscular Disease, Yonsei University College of Medicine, Seoul 135-720, Korea. kswoong@yuhs.ac
- 2Department of Rehabilitation Medicine, Wonkwang University College of Medicine, Iksan 570-711, Korea.
- KMID: 2266790
- DOI: http://doi.org/10.5535/arm.2012.36.1.126
Abstract
OBJECTIVE
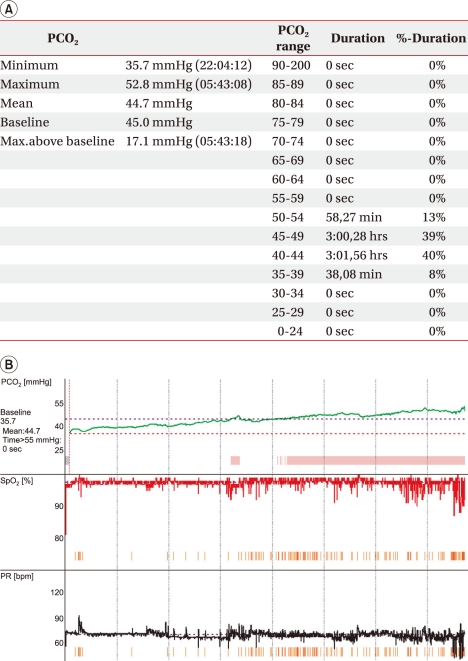
To reveal the significance of continuous transcutaneous carbon dioxide (CO2) level monitoring through reviewing cases which showed a discrepancy in CO2 levels between arterial blood gas analysis (ABGA) and continuous transcutaneous blood gas monitoring. METHOD: Medical record review was conducted retrospectively of patients with neuromuscular diseases who had started home mechanical ventilation between June 2008 and May 2010. The 89 patients underwent ABGA at the 1st hospital day, and changes to their CO2 level were continuously monitored overnight with a transcutaneous blood gas analysis device. The number of patients who initially appeared to show normal PaCO2 through ABGA, yet displayed hypercapnea through overnight continuous monitoring, was counted.
RESULTS
36 patients (40.45%) presented inconsistent CO2 level results between ABGA and continuous overnight monitoring. The mean CO2 level of the 36 patients using ABGA was 37.23+/-5.11 mmHg. However, the maximum and mean CO2 levels from the continuous monitoring device were 52.25+/-6.87 mmHg and 46.16+/-6.08 mmHg, respectively. From the total monitoring period (357.28+/-150.12 minutes), CO2 retention over 45 mmHg was detected in 198.97 minutes (55.69%).
CONCLUSION
Although ABGA only reflects ventilatory status at the puncturing moment, ABGA results are commonly used to monitor ventilatory status in most clinical settings. In order to decide the starting point of home mechanical ventilation in neuromuscular patients, continuous overnight monitoring should be considered to assess latent CO2 retention.
Keyword
MeSH Terms
Figure
Reference
-
1. Dorrington KL, Balanos GM, Talbot NP, Robbins PA. Extent to which pulmonary vascular responses to PCO2 and PO2 play a functional role within the healthy human lung. J Appl Physiol. 2010; 108:1084–1096. PMID: 20185627.2. Bolliger D, Steiner LA, Kasper J, Aziz OA, Filipovic M, Seeberger MD. The accuracy of non-invasive carbon dioxide monitoring: a clinical evaluation of two transcutaneous systems. Anaesthesia. 2007; 62:394–399. PMID: 17381578.
Article3. Akai L, Ishizaki S, Matsuoka M, Homma I. Characteristics of respiratory pattern and anxiety in rhythmic gymnasts. Adv Exp Med Biol. 2010; 669:329–332. PMID: 20217376.
Article4. Masaoka Y, Homma I. Anxiety and respiratory patterns: their relationship during mental stress and physical load. Int J Psychophysiol. 1997; 27:153–159. PMID: 9342646.
Article5. Pfaltz MC, Grossman P, Michael T, Margraf J, Wilhelm FH. Physical activity and respiratory behavior in daily life of patients with panic disorder and healthy controls. Int J Psychophysiol. 2010; 78:42–49. PMID: 20472006.
Article6. Storre JH, Magnet FS, Dreher M, Windisch W. Transcutaneous monitoring as a replacement for arterial PCO2 monitoring during nocturnal non-invasive ventilation. Respir Med. 2011; 105:143–150. PMID: 21030230.7. Janssens JP, Howarth Frey C, Chevrolet JC, Abajo B, Rochat T. Transcutaneous PCO2 to monitor noninvasive mechanical ventilation in adults: assessment of a new transcutaneous PCO2 device. Chest. 1998; 113:768–773. PMID: 9515855.8. Bach J, Alba A. Noninvasive options for ventilatory support of the traumatic high level quadriplegic patient. Chest. 1990; 98:613–619. PMID: 2203616.
Article9. Kang SW. Pulmonary rehabilitation in patients with neuromuscular disease. Yonsei Med J. 2006; 47:307–314. PMID: 16807978.
Article10. Choi WA, Kang SW, Shin JC, Lee DY, Kim DH, Kim SD. Noninvasive respiratory management for patients with cervical spinal cord injury. J Korean Acad Rehabil Med. 2010; 34:518–523.11. Kang SW, Choi YC. Park CI, Moon JH, editors. Rehabilitation of Neuromuscular disease. Rehabilitation medicine. 2007. Seoul: Hanmi;p. 672.12. Brogan TV, Hedges RG, McKinney S, Robertson HT, Hlastala MP, Swenson ER. Pulmonary NO synthase inhibition and inspired CO2: effects on V'/Q' and pulmonary blood flow distribution. Eur Respir J. 2000; 16:288–295. PMID: 10968505.13. Epstein SK. Late complications of tracheostomy. Respir Care. 2005; 50:542–549. PMID: 15807919.14. Kang SW. Pulmonary rehabilitation in patients with neuromuscular disease. Yonsei Med J. 2006; 47:307–314. PMID: 16807978.
Article15. Larson CP Jr, Vender J, Seiver A. Multisite evaluation of a continuous intraarterial blood gas monitoring system. Anesthesiology. 1994; 81:543–552. PMID: 8092498.
Article16. Bussotti M, Magri D, Previtali E, Farina S, Torri A, Matturri M, Agostoni P. End-tidal pressure of CO2 and exercise performance in healthy subjects. Eur J Appl Physiol. 2008; 103:727–732. PMID: 18521623.17. Liu J, Simpson MD, Yan J, Allen R. Tracking time-varying cerebral autoregulation in response to changes in respiratory PaCO2. Physiol Meas. 2010; 31:1291–1307. PMID: 20720290.18. Vieillard-Baron A, Prin S, Augarde R, Desfonds P, Page B, Beauchet A, Jardin F. Increasing respiratory rate to improve CO2 clearance during mechanical ventilation is not a panacea in acute respiratory failure. Crit Care Med. 2002; 30:1407–1412. PMID: 12130953.19. Hazenberg A, Zijlstra JG, Kerstjens HA, Wijkstra PJ. Validation of a transcutaneous CO2 monitor in adult patients with chronic respiratory failure. Respiration. 2011; 81:242–246. PMID: 21242669.
Article20. Hinkelbein J, Floss F, Denz C, Krieter H. Accuracy and precision of three different methods to determine PCO2 (PaCO2 vs. PetCO2 vs. PtcCO2) during interhospital ground transport of critically ill and ventilated adults. J Trauma. 2008; 65:10–18. PMID: 18580512.21. Janssens JP, Perrin E, Bennani I, de Muralt B, Titelion V, Picaud C. Is continuous transcutaneous monitoring of PCO2 (TcPCO2) over 8 h reliable in adults? Respir Med. 2001; 95:331–335. PMID: 11392572.22. Nilsson E, Lagercrantz H. Validity of transcutaneous PO2 monitoring as compared with intra-arterial PO2 monitoring in newborn infants. Lancet. 1982; 1:1241. PMID: 6122991.23. Rosner V, Hannhart B, Chabot F, Polu JM. Validity of transcutaneous oxygen/carbon dioxide pressure measurement in the monitoring of mechanical ventilation in stable chronic respiratory failure. Eur Respir J. 1999; 13:1044–1047. PMID: 10414402.
Article24. Storre JH, Steurer B, Kabitz HJ, Dreher M, Windisch W. Transcutaneous PCO2 monitoring during initiation of noninvasive ventilation. Chest. 2007; 132:1810–1816. PMID: 18079217.25. Kocher S, Rohling R, Tschupp A. Performance of a digital PCO2/SPO2 ear sensor. J Clin Monit Comput. 2004; 18:75–79. PMID: 15362268.26. Mahutte CK, Michiels TM, Hassell KT, Trueblood DM. Evaluation of a single transcutaneous PO2-PCO2 sensor in adult patients. Crit Care Med. 1984; 12:1063–1066. PMID: 6439472.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Ventilatory Insufficiency in Neuromuscular Patients Using Mechanical Ventilator Supported by the Korean Government
- A study of the use of home mechanical ventilator and medical insurance
- Non-invasive Mechanical Ventilator Care for the Patients with Advanced Neuromuscular Disease
- Transcutaneous Monitoring of PO2 and PCO2 during General Anesthesia in Adult Patient
- Unusual Prolonged Recovery of Succinylcholine - induced Neuromuscular Block Following Neostigmin