Ann Rehabil Med.
2012 Jun;36(3):356-364. 10.5535/arm.2012.36.3.356.
Effect of Decannulation on Pharyngeal and Laryngeal Movement in Post-Stroke Tracheostomized Patients
- Affiliations
-
- 1Department and Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul 120-752, Korea. kimdy@yuhs.ac
- 2Department of Otorhinolaryngology Medicine, Yonsei University College of Medicine, Seoul 120-752, Korea.
- 3Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul 120-752, Korea.
- KMID: 2266741
- DOI: http://doi.org/10.5535/arm.2012.36.3.356
Abstract
OBJECTIVE
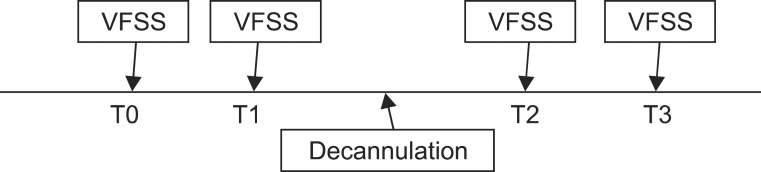
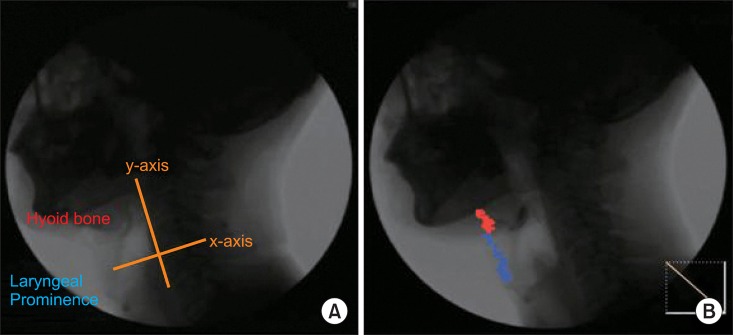
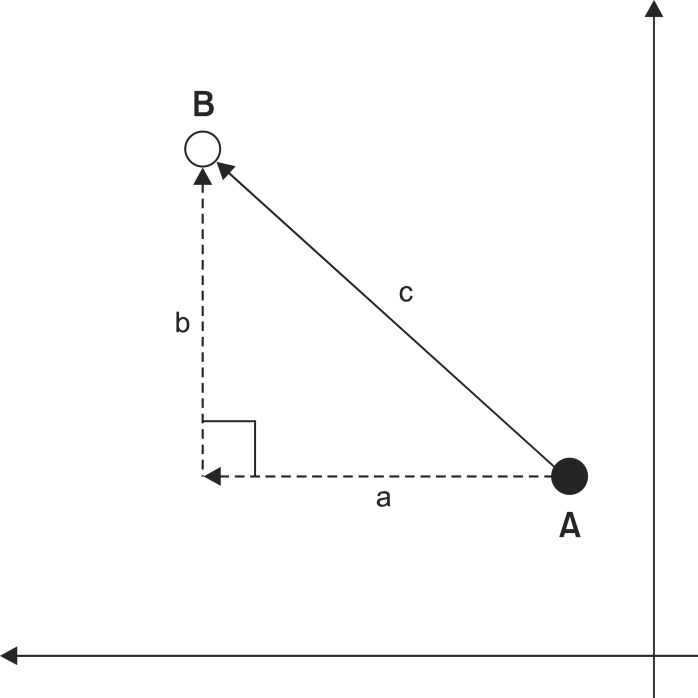
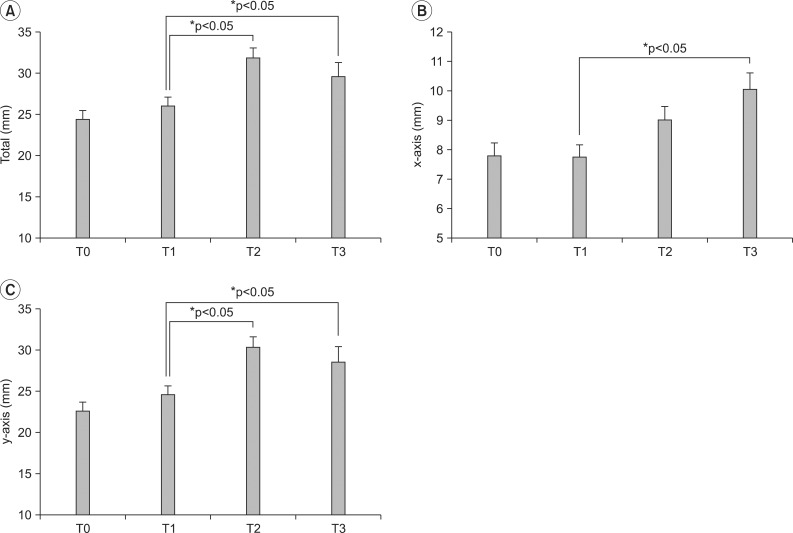
To investigate effects of tracheostomy tube on the movement of the hyoid bone and larynx during swallowing by quantitative analysis of videofluoroscopic swallowing study. METHOD: 19 adult stroke patients with tracheostomies, who met the criteria of decannulation participated. Serial videofluroscopic swallowing studies were done over 14 days before decannulation, within 24 hours before decannulation, within 24 hours after decannulation, and over 14 days after decannulation. The kinematic parameter such as pharyngeal transition time, stage transition duration, maximal hyoid bone movement, and maximal laryngeal prominence movement were obtained by 2-D quantitative analysis of videofluoroscopic swallowing study.
RESULTS
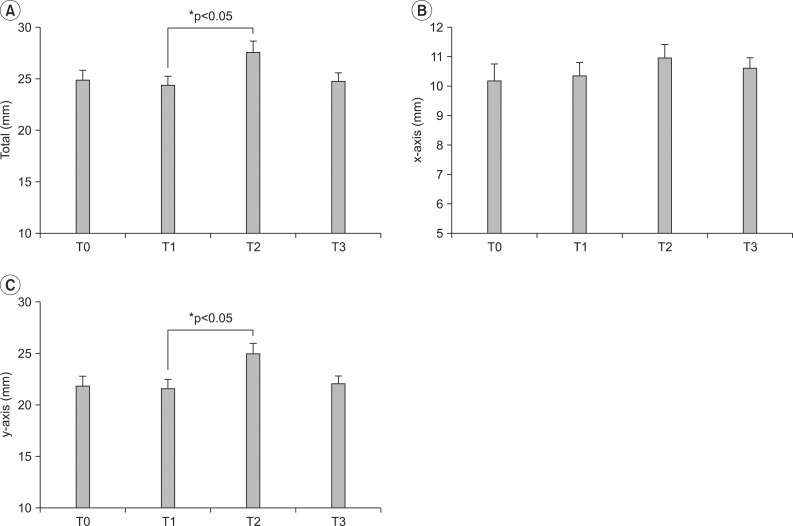
Pharyngeal transition time and stage transition duration were not significantly changed all the time. The maximal hyoid bone movement and maximal laryngeal prominence just after decannulation were improved significantly compared to just before decannulation (p<0.05), especially on vertical movement.
CONCLUSION
The hypothesis that a tracheostomy tube disturbs the hyoid bone and laryngeal movement during swallowing may be supported by this study.
Keyword
Figure
Reference
-
1. Frutos-Vivar F, Esteban A, Apezteguia C, Anzueto A, Nightingale P, Gonzalez M, Soto L, Rodrigo C, Raad J, David CM, et al. Outcome of mechanically ventilated patients who require a tracheostomy. Crit Care Med. 2005; 33:290–298. PMID: 15699830.
Article2. Kollef MH, Ahrens TS, Shannon W. Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med. 1999; 27:1714–1720. PMID: 10507588.
Article3. Nash M. Swallowing problems in the tracheostomized patient. Otolaryngol Clin North Am. 1988; 21:701–709. PMID: 3054721.4. McCulloch TM, Jaffe D, Hoffman HT. Perlman AL, Schulze-Delriew KS, editors. Diseases and operation of head and neck structures affecting swallowing. Deglutition and its disorders. 1997. 1st ed. San Diego: Singular Publishing Group Inc;p. 343–381.5. Cameron JL, Reynolds J, Zuidema GD. Aspiration in patients with tracheotomies. Surg Gynecol Obstet. 1973; 136:68–70. PMID: 4682266.6. Elpern EH, Scott MG, Petro L, Ries MH. Pulmonary aspiration in mechanically ventilated patients with tracheostomies. Chest. 1994; 105:563–566. PMID: 8306764.
Article7. Tolep K, Getch CL, Criner GJ. Swallowing dysfunction in patients receiving prolonged mechanical ventilation. Chest. 1996; 109:167–172. PMID: 8549181.
Article8. O'Connor HH, White AC. Tracheostomy decannulation. Respir Care. 2010; 55:1076–1081. PMID: 20667155.9. Smith-Hammond CA, Goldstein LB. Cough and aspiration of food and liquids due to oral-pharyngeal dysphagia: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129(Suppl 1):S154–S168.10. Bonanno PC. Swallowing dysfunction after tracheostomy. Ann Surg. 1971; 174:29–33. PMID: 5092509.
Article11. Ding R, Logemann JA. Swallow physiology in patients with trach cuff inflated or deflated: a retrospective study. Head Neck. 2005; 27:809–813. PMID: 16086414.
Article12. DeVita MA, Spierer-Rundback L. Swallowing disorders in patients with prolonged orotracheal intubation or tracheostomy tubes. Crit Care Med. 1990; 18:1328–1330. PMID: 2245604.
Article13. Higgins DM, Maclean JC. Dysphagia in the patient with a tracheostomy: six cases of inappropriate cuff deflation or removal. Heart Lung. 1997; 26:215–220. PMID: 9176689.
Article14. Suiter DM, McCullough GH, Powell PW. Effects of cuff deflation and one-way tracheostomy speaking valve placement on swallow physiology. Dysphagia. 2003; 18:284–292. PMID: 14571334.
Article15. Terk AR, Leder SB, Burrell MI. Hyoid bone and laryngeal movement dependent upon presence of a tracheotomy tube. Dysphagia. 2007; 22:89–93. PMID: 17287926.
Article16. Gross RD, Mahlmann J, Grayhack JP. Physiologic effects of open and closed tracheostomy tubes on the pharyngeal swallow. Ann Otol Rhinol Laryngol. 2003; 112:143–152. PMID: 12597287.
Article17. Hiiemae KM, Palmer JB, Medicis SW, Hegener J, Jackson BS, Lieberman DE. Hyoid and tongue surface movements in speaking and eating. Arch Oral Biol. 2002; 47:11–27. PMID: 11743928.
Article18. Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia. 2002; 17:262–272. PMID: 12355141.
Article19. Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. J Speech Lang Hear Res. 2000; 43:1264–1274. PMID: 11063246.
Article20. Kim SJ, Lee KJ. Comparison of the hyoid movement during the pharyngolaryngeal swallowing at the healthy young and old person. J Korean Acad Rehabil Med. 2006; 30:485–490.21. Wesling M, Brady S, Jensen M, Nickell M, Statkus D, Escobar N. Dysphagia outcomes in patients with brain tumors undergoing inpatient rehabilitation. Dysphagia. 2003; 18:203–210. PMID: 14506986.
Article22. Giacino JT, Kalmar K. Comarecoveryscale-revised-administration and scoring guidelines. 2004. 1st ed. New Jersey: Solaris Health System;p. 1–15.23. Kendall KA, McKenzie S, Leonard RJ, Goncalves MI, Walker A. Timing of events in normal swallowing: a videofluoroscopic study. Dysphagia. 2000; 15:74–83. PMID: 10758189.
Article24. Muz J, Mathog RH, Nelson R, Jones LA Jr. Aspiration in patients with head and neck cancer and tracheostomy. Am J Otolaryngol. 1989; 10:282–286. PMID: 2764241.
Article25. Cha DY, Yang HS, Noh JY, Lee SY, Choi JY, Kim SN, Park YO. Effect of tracheostomy tube on swallowing in patients with stroke. J Korean Acad Rehabil Med. 2010; 34:128–133.26. Dodds WJ, Stewart ET, Logemann JA. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990; 154:953–963. PMID: 2108569.
Article27. Dodds WJ, Logemann JA, Stewart ET. Radiologic assessment of abnormal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990; 154:965–974. PMID: 2108570.
Article28. Elpern EH, Scott MG, Petro L, Ries MH. Pulmonary aspiration in mechanically ventilated patients with tracheostomies. Chest. 1994; 105:563–566. PMID: 8306764.
Article29. Logemann JA. Evaluation and treatment of swallowing disorders. 1983. 1st ed. San diego: College-Hill Press Inc;p. 38–50.30. Buckwalter JA, Sasaki CT. Effect of tracheotomy on laryngeal function. Otolaryngol Clin North Am. 1984; 17:41–48. PMID: 6718024.
Article31. Logemann JA, Pauloski BR, Colangelo L. Light digital occlusion of the tracheostomy tube: a pilot study of effects on aspiration and biomechanics of the swallow. Head Neck. 1998; 20:52–57. PMID: 9464952.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improved Dysphagia After Decannulation of Tracheostomy in Patients With Brain Injuries
- The Effect of Balloon Dilatation through Video-Fluoroscopic Swallowing Study (VFSS) in Stroke Patients with Cricopharyngeal Dysfunction
- Pattern of Post-Stroke Swallowing Disorder according to the Brain Lesion
- Movement Disorders Following Cerebrovascular Lesions: Etiology, Treatment Options and Prognosis
- The Effect of Neck Posture in Swallowing of Stroke Patients