Ann Rehabil Med.
2013 Feb;37(1):133-137. 10.5535/arm.2013.37.1.133.
Spinal Accessory Neuropathy Associated With the Tumor Located on the Jugular Foramen
- Affiliations
-
- 1Department of Rehabilitation Medicine, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea. shimo.yang@gmail.com
- KMID: 2266662
- DOI: http://doi.org/10.5535/arm.2013.37.1.133
Abstract
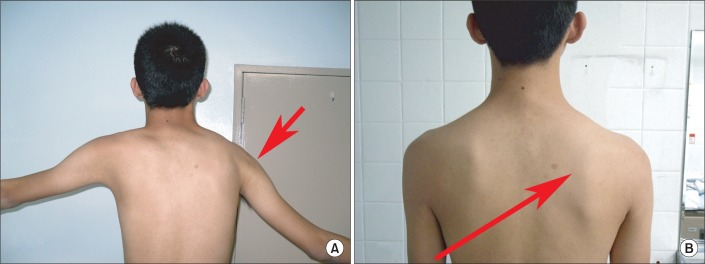
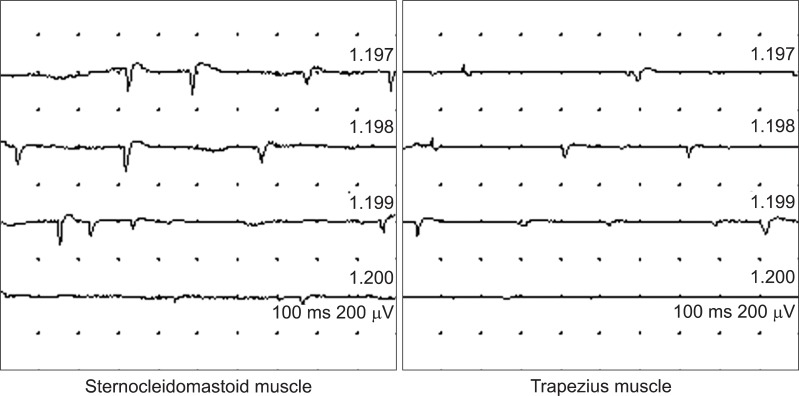
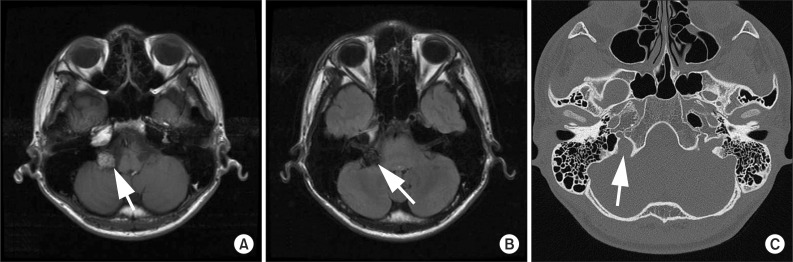
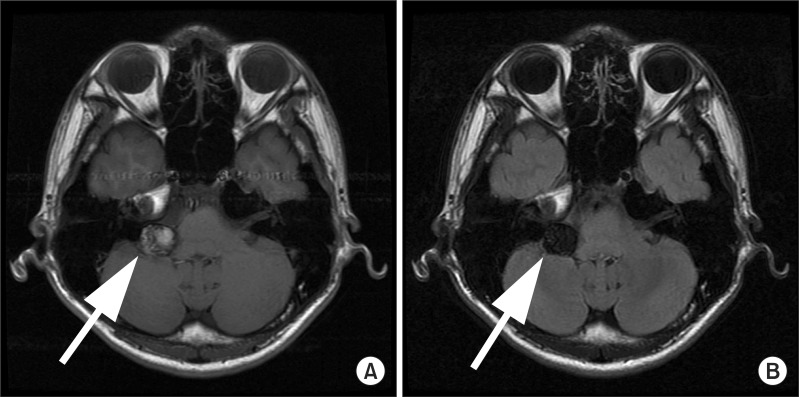
- Spinal accessory neuropathy is commonly caused by iatrogenic injury or secondary to trauma or infection. Nevertheless, the tumor related palsy is rare. We present a case of an 18-year-old male patient suffering from paralysis of his right trapezius and sternocleidomastoid muscle. An electrophysiologic diagnostic study confirmed the spinal accessory neuropathy of the proximal segment. In addition, magnetic resonance imaging showed the location of tumor on the jugular foramen. However, the type of the tumor was not confirmed through biopsy because the patient refused surgical procedure. Based on the study, it is hypothesized that the tumor located on the jugular foramen should be considered as a cause of the spinal accessory nerve of the proximal segment.
Keyword
MeSH Terms
Figure
Reference
-
1. Friedenberg SM, Zimprich T, Harper CM. The natural history of long thoracic and spinal accessory neuropathies. Muscle Nerve. 2002; 25:535–539. PMID: 11932971.
Article2. Vandeweyer E, Goldschmidt D, de Fontaine S. Traumatic spinal accessory nerve palsy. J Reconstr Microsurg. 1998; 14:259–261. PMID: 9618093.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Jugular foramen neurilemmoma mimicking an intra-axial brainstem tumor: a case report
- Delayed Spinal Accessory Neuropathy Diagnosed after Local Operative Surgical Procedures in The Posterior Cervical Triangle
- The Jugular Foramen Schwannomas: Review of the Large Surgical Series
- A Fatal Complication Associated with Combined Posterior Petrous and Suboccipital Approach to a Giant Jugular Foramen Schwannoma
- Intracisternal Cranial Root Accessory Nerve Schwannoma Associated with Recurrent Laryngeal Neuropathy