Ann Dermatol.
2012 Nov;24(4):383-392. 10.5021/ad.2012.24.4.383.
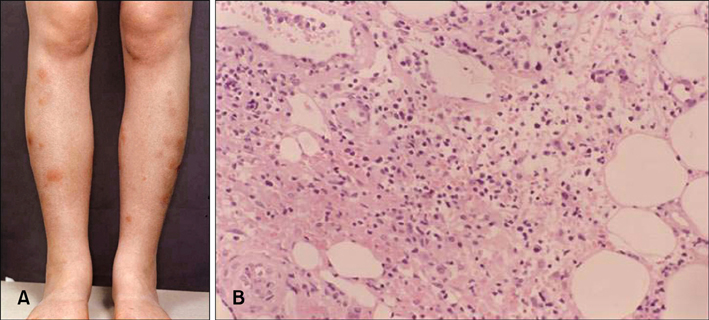
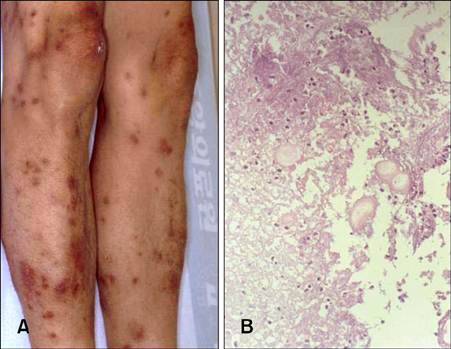
Inflammatory Nodules of the Leg
- Affiliations
-
- 1Department of Dermatology, Seoul National University College of Medicine, Seoul, Korea. khcho@snu.ac.kr
- KMID: 2266031
- DOI: http://doi.org/10.5021/ad.2012.24.4.383
Abstract
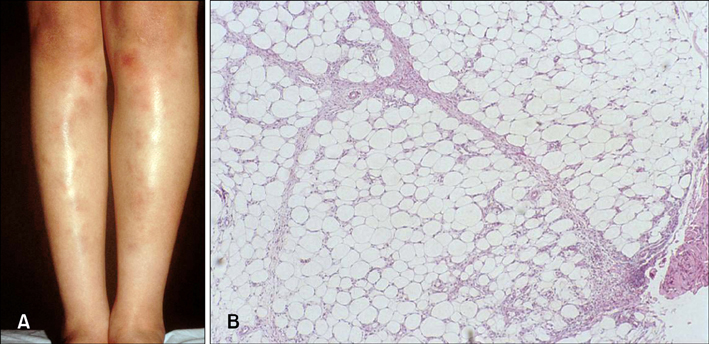
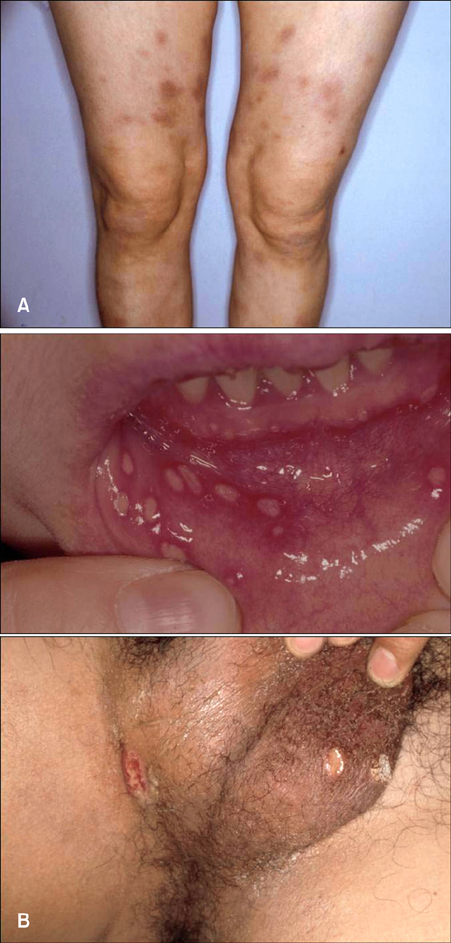
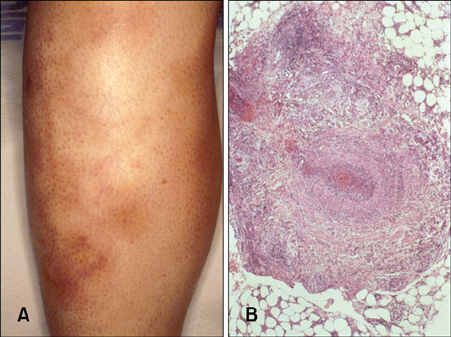
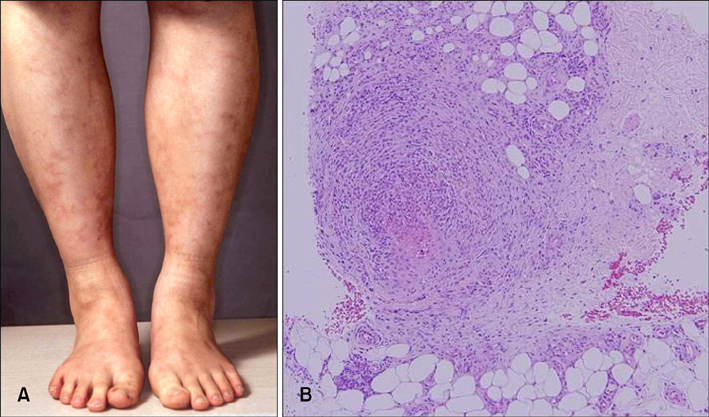
- There is a group of diseases characterized by inflammatory nodules which generally located on the lower leg. They have certain clinical appearances in common, which often makes a differential diagnosis difficult or impossible on clinical grounds alone. There is a great variation in histopathologic appearance, which depends on the duration of the lesions and sites from specimens are obtained for biopsy. Therefore, separating and subclassifying inflammatory nodule lesions of the legs, based on the subtle clinical and histological variation, is not easy. Despite all these difficulties, a specific diagnosis can be made with an adequate clinic-pathologic correlation.
Keyword
MeSH Terms
Figure
Reference
-
1. Perniciaro C, Zalla MJ, White JW Jr, Menke DM. Subcutaneous T-cell lymphoma. Report of two additional cases and further observations. Arch Dermatol. 1993. 129:1171–1176.
Article2. Fine RM, Meltzer HD. Chronic erythema nodosum. Arch Dermatol. 1969. 100:33–38.
Article3. Hannuksela M. Erythema nodosum migrans. Acta Derm Venereol. 1973. 53:313–317.4. Vilanova X, Pinol Aguade J. Subacute nodular migratory panniculitis. Br J Dermatol. 1959. 71:45–50.
Article5. Montgomery H, O'Leary PA, Barker NW. Nodular vascular diseases of the legs: erythema induratum and allied conditions. JAMA. 1945. 128:335–341.6. Darier MJ. Des "tuberculides" cutanees. Arch Dermatol Syphilol. 1896. 7:1431–1436.7. Penneys NS, Leonardi CL, Cook S, Blauvelt A, Rosenberg S, Eells LD, et al. Identification of Mycobacterium tuberculosis DNA in five different types of cutaneous lesions by the polymerase chain reaction. Arch Dermatol. 1993. 129:1594–1598.
Article8. Won YH, Oh JS, Park K, Chun IK. Detection of Mycobacterium tuberculosis from paraffinembedded tissues of skin tuberculosis by nested - polymerase chain reaction. Korean J Dermatol. 1996. 34:64–70.9. Mascaró JM Jr, Baselga E. Erythema induratum of bazin. Dermatol Clin. 2008. 26:439–445.
Article10. Angus J, Roberts C, Kulkarni K, Leach I, Murphy R. Usefulness of the QuantiFERON test in the confirmation of latent tuberculosis in association with erythema induratum. Br J Dermatol. 2007. 157:1293–1294.
Article11. Ji JH, Park H, Lee YH, Lee HJ, Choi EH. Application of the QuantiFERON(R)-TB Gold test in two cases of erythema induratum of Bazin. Korean J Dermatol. 2009. 47:850–854.12. Cho KH, Lee DY, Kim CW. Erythema induratum of Bazin. Int J Dermatol. 1996. 35:802–808.13. Segura S, Pujol RM, Trindade F, Requena L. Vasculitis in erythema induratum of Bazin: a histopathologic study of 101 biopsy specimens from 86 patients. J Am Acad Dermatol. 2008. 59:839–851.
Article14. Schneider JW, Jordaan HF. The histopathologic spectrum of erythema induratum of Bazin. Am J Dermatopathol. 1997. 19:323–333.
Article15. Cribier B, Caille A, Heid E, Grosshans E. Erythema nodosum and associated diseases. A study of 129 cases. Int J Dermatol. 1998. 37:667–672.
Article16. Yang SG, Han KH, Cho KH, Lee AY. Development of erythema nodosum in the course of oestrogen replacement therapy. Br J Dermatol. 1997. 137:319–320.17. Chun SI, Su WP, Lee S, Rogers RS 3rd. Erythema nodosum-like lesions in Behçet's syndrome: a histopathologic study of 30 cases. J Cutan Pathol. 1989. 16:259–265.
Article18. Kim B, LeBoit PE. Histopathologic features of erythema nodosum--like lesions in Behçet disease: a comparison with erythema nodosum focusing on the role of vasculitis. Am J Dermatopathol. 2000. 22:379–390.
Article19. Horio T, Imamura S, Danno K, Ofuji S. Potassium iodide in the treatment of erythema nodosum and nodular vasculitis. Arch Dermatol. 1981. 117:29–31.
Article20. Samlaska CP, James WD. Superficial thrombophlebitis. II. Secondary hypercoagulable states. J Am Acad Dermatol. 1990. 23:1–18.
Article21. Requena L, Yus ES, Kutzner H. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Panniculitis. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;569–585.22. Morgan AJ, Schwartz RA. Cutaneous polyarteritis nodosa: a comprehensive review. Int J Dermatol. 2010. 49:750–756.
Article23. Yeon JH, Kim BY, Park KC, Cho KH. Five cases of cutaneous polyarteritis nodosa treated with dapsone. Korean J Dermatol. 2008. 46:1240–1244.24. Cho KH, Oh JK, Kim CW, Heo DS, Kim ST. Peripheral T-cell lymphoma involving subcutaneous tissue. Br J Dermatol. 1995. 132:290–295.
Article25. Cho KH, Choi WW, Youn CS, Kim CW, Heo DS. Skin is the frequent site for involvement of peripheral T-cell and natural killer cell lymphomas in Korea. J Dermatol. 2000. 27:500–507.
Article26. Cho K, Kim C, Yang S, Kim B, Kim J. Angiocentric T cell lymphoma of the skin presenting as inflammatory nodules of the leg. Clin Exp Dermatol. 1997. 22:104–108.
Article27. Lee DW, Yang JH, Lee SM, Won CH, Chang S, Lee MW, et al. Subcutaneous panniculitis-like T-cell lymphoma: a clinical and pathologic study of 14 Korean patients. Ann Dermatol. 2011. 23:329–337.
Article28. Luzar B, Calonje E. Calonje E, Brenn T, Lazar A, McKee PH, editors. Inflammatory disease of the subcutaneous fat. McKee's pathology of the skin. 2012. 4th ed. Philadelphia: Elsevier;326–361.29. Moon SE. A clinical and pathological study of sarcoidosis. Korean J Dermatol. 1995. 33:922–930.30. Cho KH, Kim YG, Yang SG, Lee DY, Chung JH. Inflammatory nodules of the lower legs: a clinical and histological analysis of 134 cases in Korea. J Dermatol. 1997. 24:522–529.
Article31. Rademaker M, Lowe DG, Munro DD. Erythema induratum (Bazin's disease). J Am Acad Dermatol. 1989. 21:740–745.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinicopathological observation of the patients with isoniazid responsive inflammatory nodules on the legs
- The Significance of Mantoux Test and Antitubercular Therapy in the Patients with Inflammatory Nodules on the Legs
- Extensive Nevus Comedonicus with Inflammatory Nodules and Cysts Controlled with Adalimumab
- A Case of Benign Multiple Pulmonary Nodules in a Patient with Osteosarcoma
- Erythema Induratum of Bazin