Ann Dermatol.
2010 May;22(2):238-240. 10.5021/ad.2010.22.2.238.
Breast Cancer Cutaneous Metastasis at Core Needle Biopsy Site
- Affiliations
-
- 1Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea. leejd@olmh.cuk.ac.kr
- 2Department of General Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2265406
- DOI: http://doi.org/10.5021/ad.2010.22.2.238
Abstract
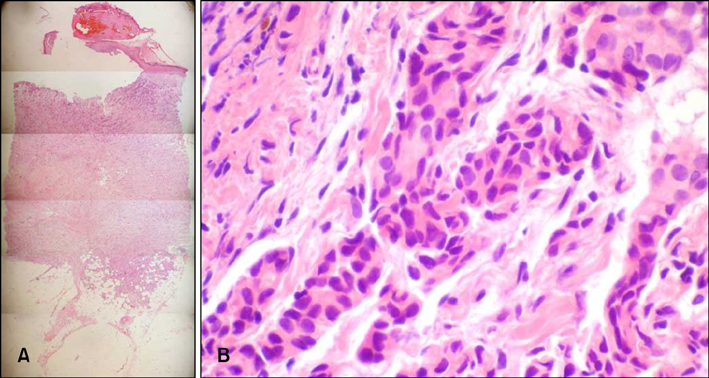
- Cutaneous metastasis from breast cancer can occur by direct invasion, lymphatic and vascular spread as well as iatrogenic implantation. Metastasis that occurs by iatrogenic implantation after needle biopsy is very rare but the potential risk must be considered. In this report, we describe a case of breast cancer cutaneous metastasis that occurred by iatrogenic implantation following core needle biopsy. A 53-year-old woman presented with a 1x1 cm sized erythematous nodule at the biopsy site after breast conserving surgery for primary cancer. Histopathological findings confirmed cutaneous metastasis. The possibility of this consequence must be considered when performing needle biopsies.
MeSH Terms
Figure
Reference
-
1. Krathen RA, Orengo IF, Rosen T. Cutaneous metastasis: a meta-analysis of data. South Med J. 2003. 96:164–167.
Article2. Kim JH, Lee MH, Haw CR. Cutaneous metastasis of pancreatic carcinoma by percutaneous fine needle aspiration biopsy. Ann Dermatol. 1995. 7:206–209.
Article3. Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol. 1993. 29:228–236.
Article4. Harter LP, Curtis JS, Ponto G, Craig PH. Malignant seeding of the needle track during stereotaxic core needle breast biopsy. Radiology. 1992. 185:713–714.
Article5. Liebens F, Carly B, Cusumano P, Van Beveren M, Beier B, Fastrez M, et al. Breast cancer seeding associated with core needle biopsies: a systematic review. Maturitas. 2009. 62:113–123.
Article6. Uematsu T, Kasami M. The use of positive core wash cytology to estimate potential risk of needle tract seeding of breast cancer: directional vacuum-assisted biopsy versus automated core needle biopsy. Breast Cancer. 2010. 17:61–67.
Article7. Chao C, Torosian MH, Boraas MC, Sigurdson ER, Hoffman JP, Eisenberg BL, et al. Local recurrence of breast cancer in the stereotactic core needle biopsy site: case reports and review of the literature. Breast J. 2001. 7:124–127.
Article8. Uriburu JL, Vuoto HD, Cogorno L, Isetta JA, Candas G, Imach GC, et al. Local recurrence of breast cancer after skin-sparing mastectomy following core needle biopsy: case reports and review of the literature. Breast J. 2006. 12:194–198.
Article9. Intra M, Mazzarol G, Rietjens M, Diaz Brito JA, Gennari R, Soteldo J, et al. Extramammary recurrence of DCIS after total mastectomy: an iatrogenic displacement following needling procedures? Breast J. 2005. 11:297–300.
Article10. Nagi C, Bleiweiss I, Jaffer S. Epithelial displacement in breast lesions: a papillary phenomenon. Arch Pathol Lab Med. 2005. 129:1465–1469.
Article11. Diaz LK, Wiley EL, Venta LA. Are malignant cells displaced by large-gauge needle core biopsy of the breast? AJR Am J Roentgenol. 1999. 173:1303–1313.
Article12. Fitzal F, Sporn EP, Draxler W, Mittlbock M, Taucher S, Rudas M, et al. Preoperative core needle biopsy does not increase local recurrence rate in breast cancer patients. Breast Cancer Res Treat. 2006. 97:9–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pseudoaneurysm of the Breast after Core Needle Biopsy: A Case Report
- Track Seeding in a Breast Cancer Patient after a 14-Gauge Core Needle Biopsy: A Case Report
- Ultrasonographic Features and the Diagnostic Role of Core Needle Biopsy at Metastatic Breast Cancer in the Thyroid gland: A Case Report
- Clinicopathologic Features of the Papillary Breast Lesions Diagnosed on Ultrasonography-guided Core Needle Biopsy
- Screening and Diagnosis for Breast Cancers