Korean J Crit Care Med.
2015 May;30(2):82-88. 10.4266/kjccm.2015.30.2.82.
Pharmacotherapeutic Problems and Pharmacist Interventions in a Medical Intensive Care Unit
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 2Department of Pharmacy, Seoul National University Hospital, Seoul, Korea. naanemone@naver.com
- KMID: 2227667
- DOI: http://doi.org/10.4266/kjccm.2015.30.2.82
Abstract
- BACKGROUND
Interest in pharmacist participation in the multidisciplinary intensive care team is increasing. However, studies examining pharmacist interventions in the medical intensive care unit (MICU) are limited in Korea. The aim of this study was to describe the current status of pharmacist interventions and to identify common pharmacologic problems requiring pharmacist intervention in the MICU.
METHODS
Between September 2013 and August 2014, a retrospective, observational study was conducted in the 22-bed MICU at a university hospital. Data were obtained from two trained pharmacists who participated in MICU rounds three times a week. In addition to patient characteristics, data on the cause, type, related drug, and acceptance rate of interventions were collected.
RESULTS
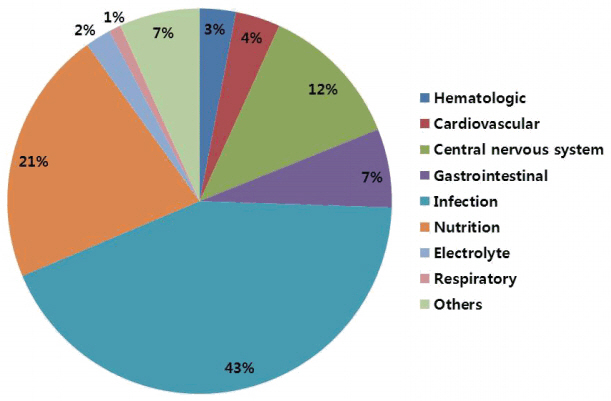
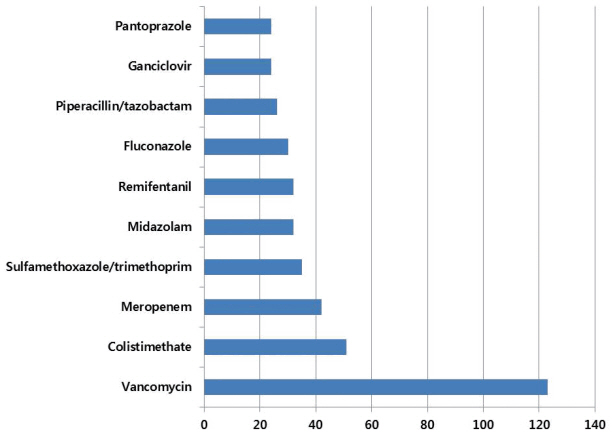
In 340 patients, a total of 1211 pharmacologic interventions were performed. The majority of pharmacologic interventions were suggested by pharmacists at multidisciplinary rounds in the MICU. The most common pharmacologic interventions were adjustment of dosage and administration (n = 328, 26.0%), followed by parenteral/enteral nutritional support (n = 228, 18.1%), the provision of drug information (n = 228, 18.1%), and advice regarding pharmacokinetics (n = 118, 9.3%). Antimicrobial agents (n = 516, 42.6%) were the most frequent type of drug associated with pharmacist interventions. The acceptance rate of interventions was 84.1% with most accepted by physicians within 24 hours (n = 602, 92.8%).
CONCLUSIONS
Medication and nutritional problems are frequently encountered pharmacotherapeutic problems in the MICU. Pharmacist interventions play an important role in the management of these problems.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Montazeri M, Cook DJ. Impact of a clinical pharmacist in a multidisciplinary intensive care unit. Crit Care Med. 1994; 22:1044–8.
Article2. Klopotowska JE, Kuiper R, van Kan HJ, de Pont AC, Dijkgraaf MG, Lie-A-Huen L, et al. On-ward participation of a hospital pharmacist in a Dutch intensive care unit reduces prescribing errors and related patient harm: an intervention study. Crit Care. 2010; 14:R174.
Article3. Kopp BJ, Mrsan M, Erstad BL, Duby JJ. Cost implications of and potential adverse events prevented by interventions of a critical care pharmacist. Am J Health Syst Pharm. 2007; 64:2483–7.
Article4. Anthes AM, Harinstein LM, Smithburger PL, Seybert AL, Kane-Gill SL. Improving adverse drug event detection in critically ill patients through intensive care unit transfer summary screening. Pharmacoepidemiol Drug Saf. 2013; 22:510–6.5. Kim JM, Park SJ, Sohn YM, Lee YM, Yang CS, Gwak HS, et al. Development of clinical pharmacy services for intensive care units in Korea. Springerplus. 2014; 3:34.
Article6. Kang M, Kim A, Cho Y, Kim H, Lee H, Yu YJ, et al. Effect of clinical pharmacist interventions on prevention of adverse drug events in surgical intensive care unit. Korean J Crit Care Med. 2013; 28:17–24.
Article7. Oh YK, Lee GS, Rhie S. Neonatal total nutritional pharmacy service at intensive care unit at a university hospital in Korea. Kor J Clin Pharm. 2013; 23:167–74.8. Craven DE, Kunches LM, Lichtenberg DA, Kollisch NR, Barry MA, Heeren TC, et al. Nosocomial infection and fatality in medical and surgical intensive care unit patients. Arch Intern Med. 1988; 148:1161–8.
Article9. Jiang SP, Chen J, Zhang XG, Lu XY, Zhao QW. Implementation of pharmacists’ interventions and assessment of medication errors in an intensive care unit of a Chinese tertiary hospital. Ther ClinRisk Manag. 2014; 10:861–6.10. Saokaew S, Maphanta S, Thangsomboon P. Impact of pharmacist’s interventions on cost of drug therapy in intensive care unit. Pharm Pract (Granada). 2009; 7:81–7.
Article11. Moyen E, Camiré E, Stelfox HT. Clinical review: medication errors in critical care. Crit Care. 2008; 12:208.
Article12. Camiré E, Moyen E, Stelfox HT. Medication errors in critical care: risk factors, prevention and disclosure. CMAJ. 2009; 180:936–43.13. Cullen DJ, Sweitzer BJ, Bates DW, Burdick E, Edmondson A, Leape LL. Preventable adverse drug events in hospitalized patients: a comparative study of intensive care and general care units. Crit Care Med. 1997; 25:1289–97.14. Kane-Gill S, Rea RS, Verrico MM, Weber RJ. Adverse-drug-event rates for high-cost and high-use drugs in the intensive care unit. Am J Health Syst Pharm. 2006; 63:1876–81.
Article15. Zaidi ST, Hassan Y, Postma MJ, Ng SH. Impact of pharmacist recommendations on the cost of drug therapy in ICU patients at a Malaysian hospital. Pharm World Sci. 2003; 25:299–302.
Article16. Kaushal R, Bates DW, Abramson EL, Soukup JR, Goldmann DA. Unit-based clinical pharmacists’ prevention of serious medication errors in pediatric inpatients. Am J Health-Syst Pharm. 2008; 65:1254–60.
Article17. Leape LL, Cullen DJ, Clapp MD, Burdick E, Demonaco HJ, Erickson JI, et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999; 282:267–70.
Article18. Agalu A, Ayele Y, Bedada W, Woldie M. Medication prescribing errors in the intensive care unit of Jimma University Specialized Hospital, Southwest Ethiopia. J Multidiscip Healthc. 2011; 4:377–82.19. Bourne RS, Choo CL. Pharmacist proactive medication recommendations using electronic documentation in a UK general critical care unit. Int J Clin Pharm. 2012; 34:351–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Clinical Pharmacist Interventions on Prevention of Adverse Drug Events in Surgical Intensive Care Unit
- Pharmacological Interventions on Surgical Intensive Care Units Initiated by Pharmacists
- Effects of Medication Reconciliation and Cost Avoidance Analysis by Clinical Pharmacists in a Neurocritical Care Unit
- Risk Factors for Cognitive Impairment in Intensive Care Unit Survivors
- Rehabilitation in Intensive Care Unit