Korean Circ J.
2009 Dec;39(12):551-555. 10.4070/kcj.2009.39.12.551.
Takayasu's Arteritis Involving the Ostia of Three Large Coronary Arteries
- Affiliations
-
- 1Department of Internal Medicine/Cardiac Catheterization Laboratory, Pusan National University Hospital, Busan, Korea. glaraone@hanmail.net
- KMID: 2225645
- DOI: http://doi.org/10.4070/kcj.2009.39.12.551
Abstract
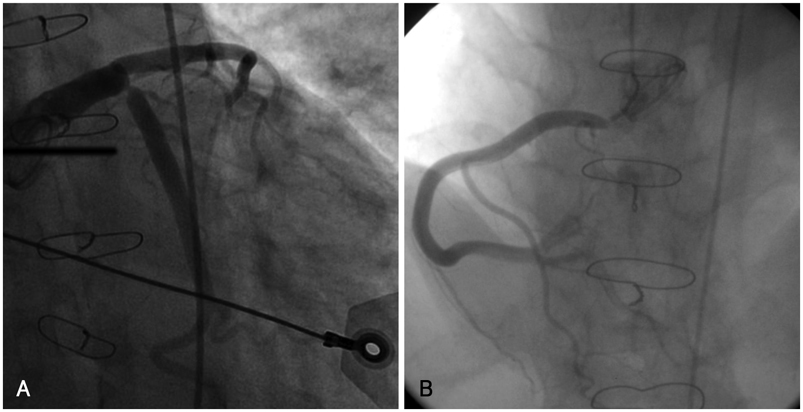
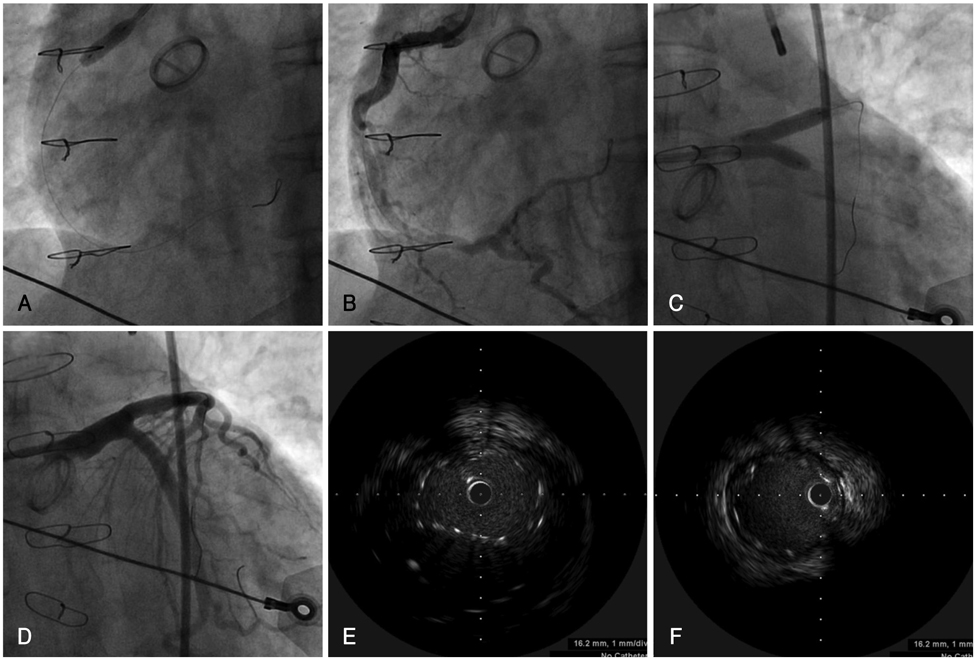
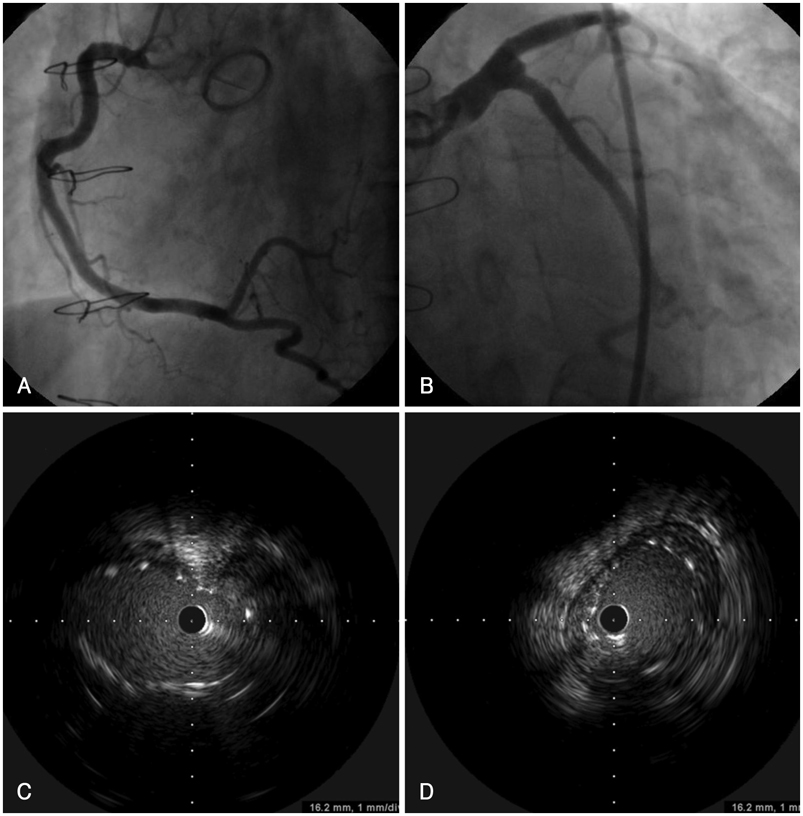
- Takayasu's arteritis can involve the ostia of coronary arteries. We report a patient with Takayasu's arteritis involving the ostia of three large coronary arteries who was successfully treated by percutaneous coronary intervention (PCI) with a drug-eluting stent (DES) and had a good clinical outcome after 12 months. A 37-year-old male with unstable angina was admitted to our cardiovascular center. The patient had Takayasu's arteritis and an aortic valve replacement with a metallic valve due to severe aortic regurgitation 7 years previously. Coronary angiography (CAG) showed a 95% discrete eccentric luminal narrowing at the ostia of the large left anterior descending (LAD) and left circumflex (LCX) arteries, and a 99% discrete eccentric luminal narrowing at the ostium of the large right coronary artery (RCA). The patient was treated with prednisolone for 14 days. Two large paclitaxel-eluting stents (PES) were then implanted in the distal left main coronary artery using the kissing stent technique. After 6 months, a CAG did not reveal restenosis or recurrent coronary artery disease. Thus, PCI with a DES for patients with significant coronary involvement secondary to Takayasu's arteritis is an effective and an alternative treatment when coronary bypass grafting is not option.
Keyword
MeSH Terms
Figure
Reference
-
1. Furukawa Y, Tamura T, Toma M, et al. Sirolimus-eluting stent for in-stent restenosis of left main coronary artery in takayasu arteritis. Circ J. 2005. 69:752–755.2. Amir O, Kar B, Civitello AB, Palanichamy N, Shakir A, Delgado RM 3rd. Unprotected left main stent placement in a patient with Takayasu's arteritis: an unusual solution for an unusual disease. Tex Heart Inst J. 2006. 33:253–255.3. Kang WC, Han SH, Oh KJ, Ahn TH, Shin EK. Images in cardiovascular medicine: implantation of a drug-eluting stent for the coronary artery stenosis of Takayasu arteritis: de novo and instent restenosis. Circulation. 2006. 113:e735–e737.4. Amano J, Suzuki A. Coronary artery involvement in Takayasu's arteritis: collective review and guideline for surgical treatment. J Thorac Cardiovasc Surg. 1991. 102:554–560.5. Endo M, Tomizawa Y, Nishida H, et al. Angiographic findings and surgical treatments of coronary artery involvement in Takayasu arteritis. J Thorac Cardiovasc Surg. 2003. 125:570–577.6. Son JW, Koh KK, Dang Q, Choi IS, Shin EK. Recurrent restenosis following stent and rotational atherectomy of coronary artery stenosis in Takayasu's arteritis. Int J Cardiol. 1998. 65:295–300.7. Malik IS, Harare O, AL-Nahhas A, Beatt K, Mason J. Takayasu's arteritis: management of left main stem stenosis. Heart. 2003. 89:e9.8. Subramanyan R, Joy J, Balakrishnan KG. Natural history of aortoarteritis (Takayasu's disease). Circulation. 1989. 80:429–437.9. Park YB, Hong SK, Choi KJ, et al. Takayasu arteritis in Korea: clinical and angiographic features. Heart Vessels Suppl. 1992. 7:55–59.10. Matsubara O, Kuwata T, Nemoto T, Kasuga T, Numano F. Coronary artery lesions in Takayasu arteritis: pathological considerations. Heart Vessels Suppl. 1992. 7:26–31.11. Amano J, Suzuki A. Coronary artery involvement in Takayasu's arteritis: collective review and guideline for surgical treatment. J Thorac Cardiovasc Surg. 1991. 102:554–560.12. Amano J, Suzuki A. Surgical treatment of cardiac involvement in Takayasu arteritis. Heart Vessels Suppl. 1992. 7:168–178.13. Chun KJ, Kim SI, Na MA, Choi JH. Bilateral ostial coronary artery lesions in a patient with Takayasu's arteritis. Korean Circ J. 2004. 34:118–119.14. Kang KT, Jeong MH, Jeong WG, et al. Long-term clinical follow-up in a case of Takayasu's arteritis involving the ostium of left coronary artery after ostioplasty. Korean Circ J. 2001. 31:246–250.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pulmonary Hypertension with Pulmonary Arteritis Diagnosed as Takayasu's Arteritis Type IV
- A Case of Bilateral Coronary Ostial Stenosis in Takayasu's Arteritis
- A Case of Takayasu's Arteritis with Bilateral Involvement of Ostial Coronary Arteries
- Takayasu's Arteritis with Ischemic Stroke Followed by Subarachnoid Hemrrhage: A Case Report
- A Case of Takayasu's Arteritis Associated with Aortic Regurgitation and Coronary Artery Involvement