Korean Circ J.
2009 Dec;39(12):525-531. 10.4070/kcj.2009.39.12.525.
Simple Method of Counterclockwise Isthmus Conduction Block by Comparing Double Potentials and Flutter Cycle Length
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Research Institute of Clinical Medicine, Chonbuk National University, Jeonju, Korea.
- 2Department of Preventive Medicine, Research Institute of Clinical Medicine, Chonbuk National University, Jeonju, Korea.
- 3Division of Cardiology, Asan Medical Center, University of Ulsan, Seoul, Korea. kjchoi@amc.seoul.kr
- KMID: 2225640
- DOI: http://doi.org/10.4070/kcj.2009.39.12.525
Abstract
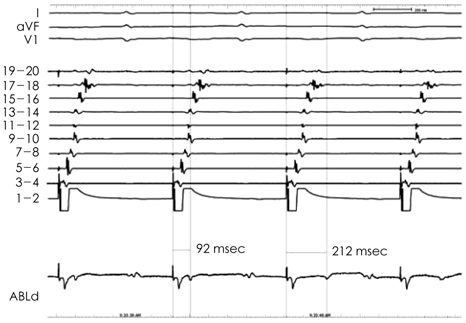
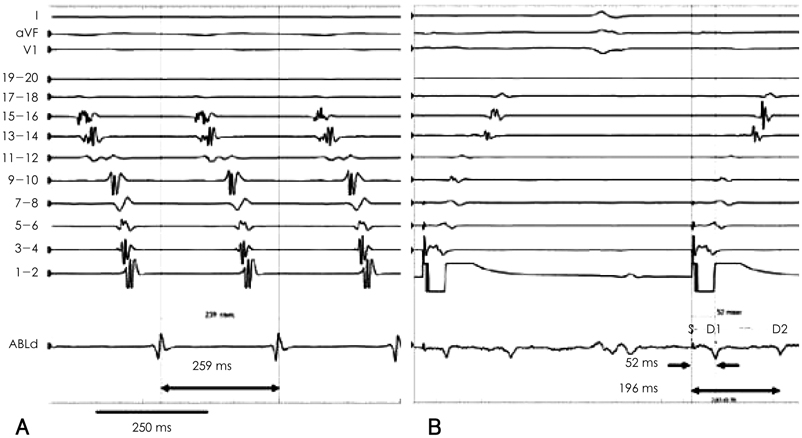
- BACKGROUND AND OBJECTIVES
Local wide split double potentials are used as a parameter to determine complete conduction block during cavotricuspid isthmus ablation in patients with isthmus dependent atrial flutter. However, delayed slow conduction in that region can sometimes be very difficult to differentiate from complete block. Flutter cycle length (FCL) can be used to confirm isthmus conduction block, because FCL is a measure of conduction time around the tricuspid annulus (TA). This study was designed to determine which degree of splitting of the local electrograms is adequate to confirm complete isthmus block, using FCL as a reference. SUBJECTS AND METHODS: Cavotricuspid isthmus (CTI) ablation was performed in fifty consecutive patients. The interval between the pacing stimulus on the lateral side of the CTI and the first component of the double potentials on the block line (SD1) corresponded to the counterclockwise conduction time. The interval between the pacing stimulus and second component (SD2) represented the clockwise conduction time to the contralateral side of the ablation line. SD1 and SD2 were measured before and after complete isthmus block. RESULTS: An SD1+SD2 reaching 90% of the FCL identified the counterclockwise isthmus conduction block with 94% sensitivity and 100% specificity. CONCLUSION: If the sum of SD1 and SD2 following isthmus ablation was close to the FCL, complete conduction block was predicted with high diagnostic accuracy and positive predictive value for at least counterclockwise conduction.
Figure
Reference
-
1. Tada H, Oral H, Sticherling C, et al. Double potentials along the ablation line as a guide to radiofrequency ablation of typical atrial flutter. J Am Coll Cardiol. 2001. 38:750–755.2. Shah D, Haissaguerre M, Takahashi A, Jais P, Hocini M, Clementy J. Differential pacing for distinguishing block from persistent conduction through an ablation line. Circulation. 2000. 102:1517–1522.3. Oral H, Sticherling C, Tada H, et al. Role of transisthmus conduction intervals in predicting bidirectional block after ablation of typical atrial flutter. J Cardiovasc Electrophysiol. 2001. 12:169–174.4. Matsushita T, Chun S, Liem LB, Friday KJ, Sung RJ. Unidirectional conduction block at cavotricuspid isthmus created by radiofrequency catheter ablation in patients with typical atrial flutter. J Cardiovasc Electrophysiol. 2002. 13:1098–1102.5. Cosío FG, Awamleh P, Pastor A, Núñez A. Determining inferior vena cava-tricuspid isthmus block after typical atrial flutter ablation. Heart Rhythm. 2005. 2:328–332.6. Kim JJ, Kim YH, Chung SS, et al. Radiofrequency catheter ablation in patients with atrial flutter. Korean Circ J. 1996. 26:605–613.7. Saoudi N, Ricard P, Rinaldi JP, Yaïci K, Darmon JP, Anselme F. Methods to determine bidirectional block of the cavotricuspid isthmus in radiofrequency ablation of typical atrial flutter. J Cardiovasc Electrophysiol. 2005. 16:801–803.8. Mangat I, Tschopp DR Jr, Yang Y, Cheng J, Keung EC, Scheinman MM. Optimizing the detection of bidirectional block across the flutter isthmus for patients with typical isthmus-dependent atrial flutter. Am J Cardiol. 2003. 91:559–564.9. Deisenhofer I, Estner H, Zrenner B, et al. Left atrial tachycardia after circumferential pulmonary vein ablation for atrial fibrillation: incidence, electrophysiological characteristics, and results of radiofrequency ablation. Europace. 2006. 8:573–582.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Atrial Flutter
- Atrial Flutter Conversion in Infants and Children Using Transesophageal Atrial Pacing
- Radiofrequency Catheter Ablation in Patients with Atrial Flutter
- Transesophageal Atrial Pacing in Atrial Flutter
- Transient Conduction Block in Vasculitic Neuropathy Caused by Churg-strauss Syndrome: Transient Conduction Block in Vasculitic Neuropathy