Korean Circ J.
2015 Jan;45(1):71-76. 10.4070/kcj.2015.45.1.71.
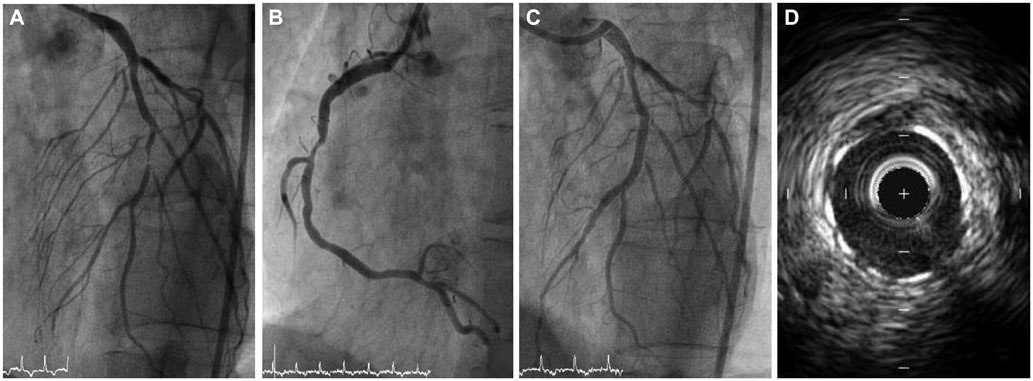
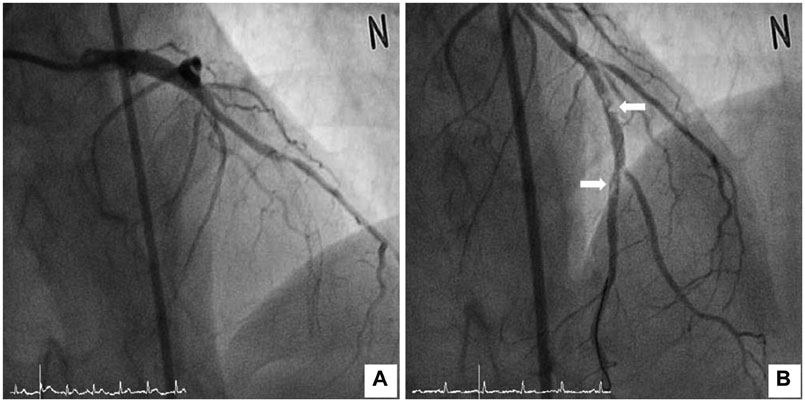
Recurrent Stent Thrombosis in a Patient with Antiphospholipid Syndrome and Dual Anti-Platelet Therapy Non-Responsiveness
- Affiliations
-
- 1Department of Cardiology, Ajou University School of Medicine, Suwon, Korea. yhhm20@hanmail.net
- 2Department of Thoracic and Cadiovascular Surgery, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2223849
- DOI: http://doi.org/10.4070/kcj.2015.45.1.71
Abstract
- Antiphospholipid syndrome (APS), the most common acquired hypercoagulable condition, is diagnosed by persistent presence of antiphospholipid antibodies and episodes of vascular thrombosis. It may be an important predisposing factor for stent thrombosis, resulting in poor outcomes. Also, anti-platelet therapy non-responsiveness is associated with stent thrombosis. We report a case of a 39-year-old man who after undergoing successful percutaneous coronary intervention for significant coronary artery disease suffered repeated stent thrombosis events leading to ST-segment elevation myocardial infarction. Eventually, he underwent coronary artery bypass surgery because of uncontrolled thrombosis and was diagnosed as having APS and dual antiplatelet therapy non-responsiveness.
MeSH Terms
Figure
Reference
-
1. Wilson WA, Gharavi AE, Koike T, et al. International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: report of an international workshop. Arthritis Rheum. 1999; 42:1309–1311.2. Takeuchi S, Obayashi T, Toyama J. Primary antiphospholipid syndrome with acute myocardial infarction recanalised by PTCA. Heart. 1998; 79:96–98.3. Ludia C, Domenico P, Monia C, et al. Antiphospholipid antibodies: a new risk factor for restenosis after percutaneous transluminal coronary angioplasty? Autoimmunity. 1998; 27:141–148.4. Van Werkum JW, Heestermans AA, Zomer AC, et al. Predictors of coronary stent thrombosis: the Dutch Stent Thrombosis Registry. J Am Coll Cardiol. 2009; 53:1399–1409.5. Miyakis S, Lockshin MD, Atsumi T, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006; 4:295–306.6. Kimura T, Morimoto T, Nakagawa Y, et al. Antiplatelet therapy and stent thrombosis after sirolimus-eluting stent implantation. Circulation. 2009; 119:987–995.7. Burzotta F, Parma A, Pristipino C, et al. Angiographic and clinical outcome of invasively managed patients with thrombosed coronary bare metal or drug-eluting stents: the OPTIMIST study. Eur Heart J. 2008; 29:3011–3021.8. Tripodi A, Chantarangkul V, Clerici M, Negri B, Galli M, Mannucci PM. Laboratory control of oral anticoagulant treatment by the INR system in patients with the antiphospholipid syndrome and lupus anticoagulant. Results of a collaborative study involving nine commercial thromboplastins. Br J Haematol. 2001; 115:672–678.9. Cervera R, Piette JC, Font J, et al. Antiphospholipid syndrome: clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. Arthritis Rheum. 2002; 46:1019–1027.10. Perl L, Netzer A, Rechavia E, et al. Long-term outcome of patients with antiphospholipid syndrome who undergo percutaneous coronary intervention. Cardiology. 2012; 122:76–82.11. Muir DF, Stevens A, Napier-Hemy RO, Fath-Ordoubadi F, Curzen N. Recurrent stent thrombosis associated with lupus anticoagulant due to renal cell carcinoma. Int J Cardiovasc Intervent. 2003; 5:44–46.12. Weissman A, Coplan NL. Antiphospholipid antibody syndrome and acute stent thrombosis. Rev Cardiovasc Med. 2006; 7:244–246.13. Middlebrooks EH, Panda M. Multiple recurrent stent thrombosis in a patient with coexisting clopidogrel resistance and increased anticardiolipin antibodies: a case report. Case Rep Med. 2010; 2010:974149.14. Musuraca G, Imperadore F, Terraneo C, et al. Successful treatment of post-exertion acute myocardial infarction by primary angioplasty and stenting in a patient with antiphospholipid antibody syndrome. Blood Coagul Fibrinolysis. 2004; 15:95–98.15. Lockshin M, Tenedios F, Petri M, et al. Cardiac disease in the antiphospholipid syndrome: recommendations for treatment. Committee consensus report. Lupus. 2003; 12:518–523.16. Levine SR, Brey RL, Tilley BC, et al. Antiphospholipid antibodies and subsequent thrombo-occlusive events in patients with ischemic stroke. JAMA. 2004; 291:576–584.17. Lim W, Crowther MA, Eikelboom JW. Management of antiphospholipid antibody syndrome: a systematic review. JAMA. 2006; 295:1050–1057.18. Klomp M, Beijk MA, Varma C, et al. 1-year outcome of TRIAS HR (TRI-stent adjudication study-high risk of restenosis) a multicenter, randomized trial comparing genous endothelial progenitor cell capturing stents with drug-eluting stents. JACC Cardiovasc Interv. 2011; 4:896–904.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiphospholipid Syndrome Associated with Adenocarcinoma
- A Case of Antiphospholipid Syndrome in A Patient with Leg Ulcer and Previous History of Deep Vein Thrombosis
- A Case of Primary Antiphospholipid Syndrome in a Patient with Diabetes Presenting as Foot Ulcer
- A Case of Leukocytoclastic Vasculitis Associated with Antiphospholipid Antibody Syndorme
- Anesthetic management of HELLP syndrome complicating primary antiphospholipid syndrome: A case report