J Korean Ophthalmol Soc.
2014 Feb;55(2):298-303. 10.3341/jkos.2014.55.2.298.
Corneal Perforation in Phlyctenular Keratitis
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, The Catholic University of Korea College of Medicine, Seoul, Korea. yangkyeung@hanmail.net
- KMID: 2218427
- DOI: http://doi.org/10.3341/jkos.2014.55.2.298
Abstract
- PURPOSE
Corneal perforation from phlyctenular keratoconjunctivitis is rarely reported worldwide and no case has been reported in Korea. We report a case of corneal perforation in a patient with phlyctenular keratoconjunctivitis along with a literature review.
CASE SUMMARY
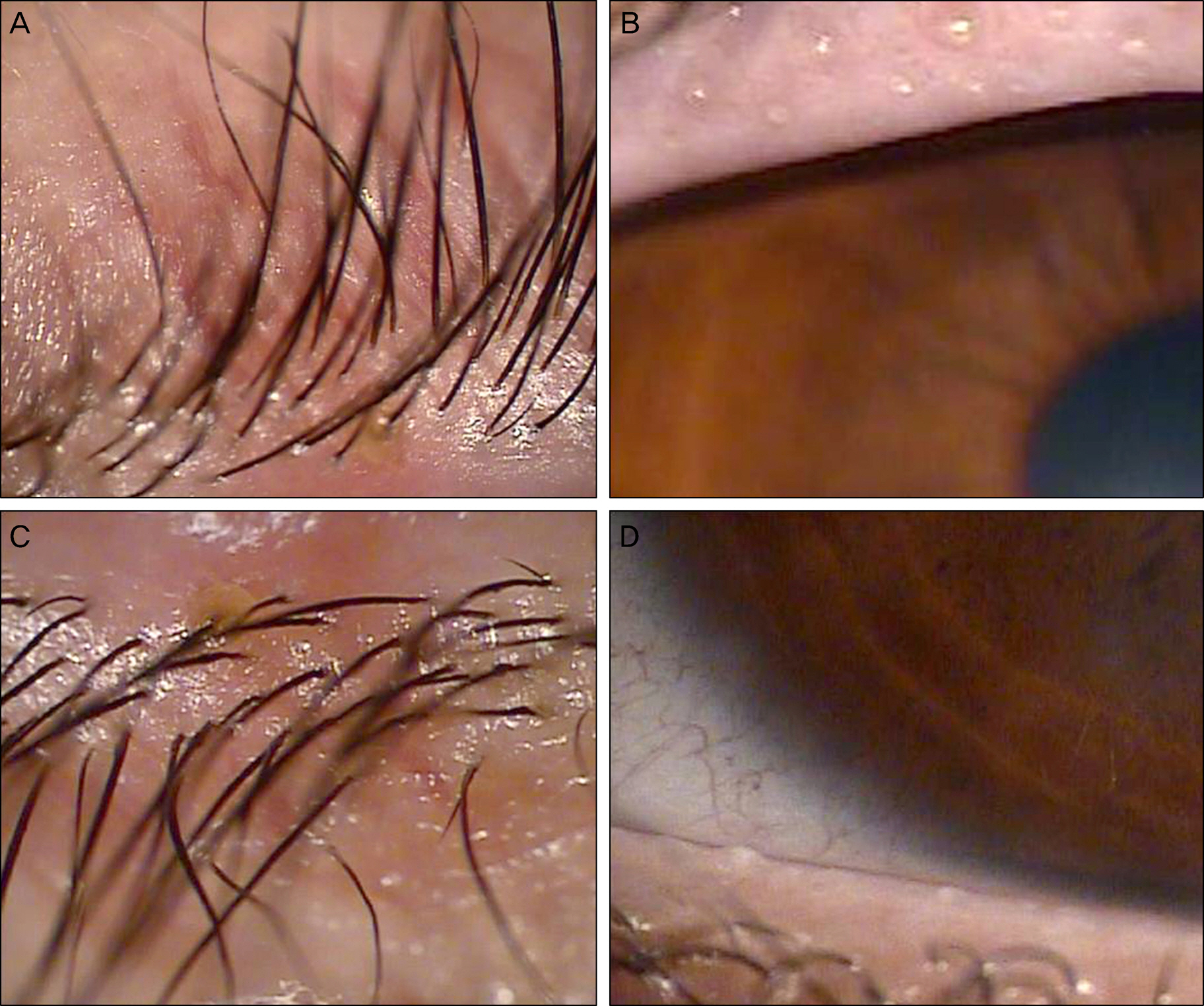
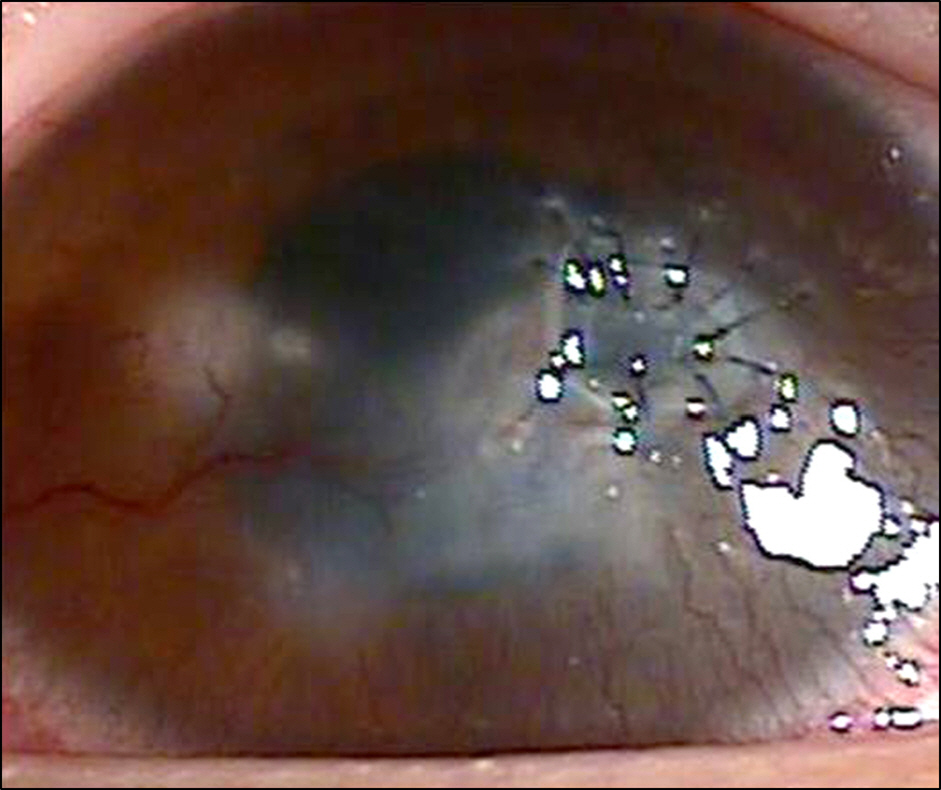
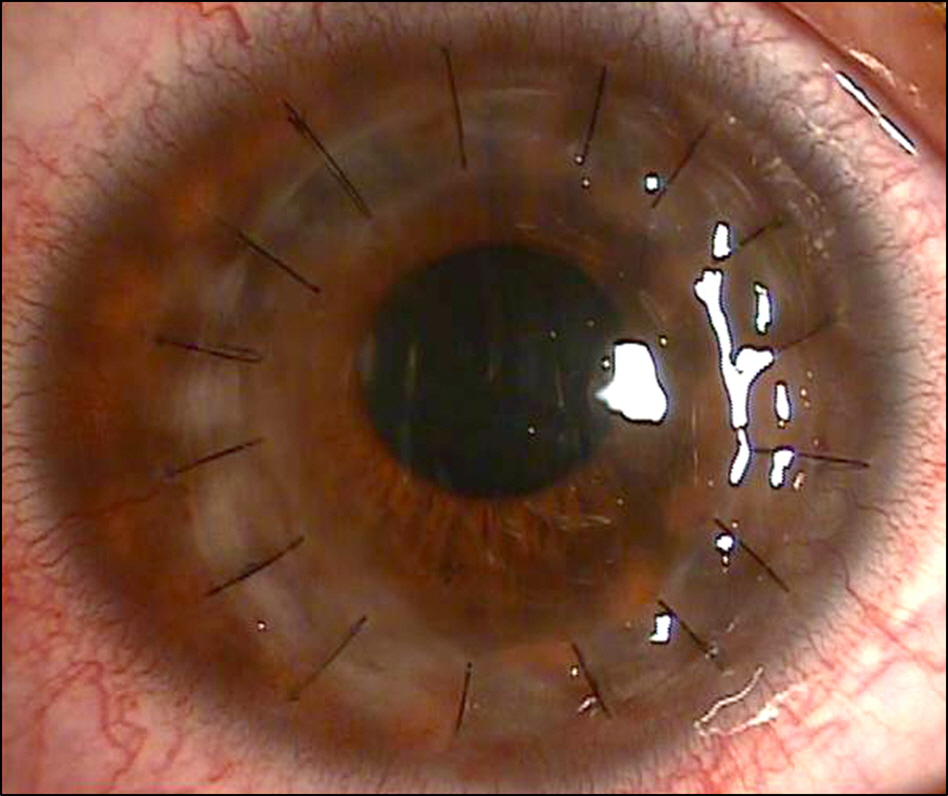
A 15-year-old female presented to our clinic with repetitive tears, conjunctival injection, and discomfort in her right eye for several months. Slit-lamp examination revealed oily plugs at the meibomian gland orifices with collarettes, conjunctival injection and a round, whitish elevated lesion accompanying neovascularization of the inferotemporal side of the cornea. As an initial treatment, topical antibiotic was given but no signs of improvement were observed. Hence, topical steroid was applied on suspicion of phlyctenular keratitis and the patient's symptoms and corneal lesion improved. Two months later, the patient's symptoms relapsed and the lesion was found progressing towards the central cornea. The treatment was restarted and the symptoms improved but the corneal lesion continuously progressed towards the center, thinning the central cornea. Seventeen months from the time of initial diagnosis, the patient revisited prior to the scheduled appointment complaining of abrupt tears in her right eye. Slit-lamp examination revealed a corneal perforation at the center of the thinned cornea. Hence, we performed an emergent tectonic corneal patch graft. After the operation, opacity remained covering the visual axis at the central cornea, thus penetrating keratoplasty was performed 10 months later. Henceforth, the patient has remained free of symptoms and visual acuity has been recovered.
CONCLUSIONS
Usually phlyctenular keratoconjunctivitis responds well to treatment and does not have a significant influence on vision. However, occasionally phlyctenular keratoconjunctivitis may not respond to treatment and may spread to the central cornea causing loss of visual acuity and even corneal perforation in rare occasions. Therefore, in order to prevent such complications, prompt diagnosis and treatment are essential.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Abu el Asrar AM, Geboes K, Maudgal PC. . Immunocytological study of phlyctenular eye disease. Int Ophthalmol. 1987; 10:33–9.
Article2. Sorsby A.The etiology of phlyctenular ophthalmia. Br J Ophthalmol. 1942; 26:189–25.3. Thygeson P.Observations on nontuberculous phlyctenular kera- toconjunctivitis. Trans Am Acad Ophthalmol Otolaryngol. 1954; 58:128–32.4. Ostler HB, Lanier JD.Phlyctenular keratoconjunctivitis with special reference to the staphylococcal type. Trans Pac Coast Otoophthalmol Soc Annu Meet. 1974; 55:237–52.5. Singal A, Aggarwal P, Pandhi D, Rohatgi J.Cutaneous tuberculosis and phlyctenular keratoconjunctivitis: a forgotten ssociation. Indian J Dermatol Venereol Leprol. 2006; 72:290–2.6. Culbertson WW, Huang AJ, Mandelbaum SH. . Effective treat-ment of phlyctenular keratoconjunctivitis with oral tetracycline. Ophthalmology. 1993; 100:1358–66.
Article7. Philip RN, Comstock GW, Shelton JH.Phlyctenular kerato-conjunctivitis among eskimos in southwestern alaska. I. epidemio-logic characteristics. Am Rev Respir Dis. 1965; 91:171–87.8. Neiberg MN, Sowka J.Phlyctenular keratoconjunctivitis in a pa-tient with Staphylococcal blepharitis and ocular rosacea. Optometry. 2008; 79:133–7.
Article9. Hussein AA, Nasr ME.The role of parasitic infection in the aetiology of phlyctenular eye disease. J Egypt Soc Parasitol. 1991; 21:865–8.10. Chung G.Phlyctenular keratoconjunctivitis and marginal staph-ylococcal keratitis. Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea. 3rd ed.St. Louis: MO Elsevier;2011. chap. 94.
Article11. Ostler HB.Corneal perforation in nontuberculous (staphylococcal) phlyctenular keratoconjunctivitis. Am J Ophthalmol. 1975; 79:446–8.
Article12. Beauchamp GR, Gillette TE, Friendly DS.Phlyctenular kera- toconjunctivitis. J Pediatr Ophthalmol Strabismus. 1981; 18:22–8.13. Thygeson P.The etiology and treatment of phlyctenular ke- ratoconjunctivitis. Am J Ophthalmol. 1951; 34:1217–36.14. Rohatgi J, Dhaliwal U.Phlyctenular eye disease: a reappraisal. Jpn J Ophthalmol. 2000; 44:146–50.
Article15. Hird RB.Phjyctenular disease and its relation to tuberculosis. Br J Ophthalmol. 1918; 2:215–23.16. Jo DH, Kim MK, Wee WR, Lee JH.Analysis of clinical character-istics in phlyctenular keratoconjunctivitis at a tertiary center. J Korean Ophthalmol Soc. 2011; 52:7–13.
Article17. Suzuki T, Mitsuishi Y, Sano Y. . Phlyctenular keratitis associated with meibomitis in young patients. Am J Ophthalmol. 2005; 140:77–82.
Article18. Mondino BJ.Inflammatory diseases of the peripheral cornea. Ophthalmology. 1988; 95:463–72.
Article19. abu el-Asrar AM, Van den Oord JJ, Geboes K. . Phenotypic characterization of inflammatory cells in phlyctenular eye disease. Doc Ophthalmol. 1988; 70:353–62.
Article20. Zaidman GW, Brown SI.Orally administered tetracycline for phl- yctenular keratoconjunctivitis. Am J Ophthalmol. 1981; 92:178–82.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Therapeutic Effects of a 0.03% Tacrolimus Ointment on Childhood Phlyctenular Keratitis
- Excimer Laser Phototherapeutic Keratectomy for Experimental Fungal Keratitis
- Therapeutic Uses of T-lens(Soflens(R)) in Corneal Diseases
- The Effects of the Cyanoacrylate Tissue Adhesive Mono-therapy for Corneal Perforation
- The Results of Cyanoacrylate Glue Application for Corneal Perforation and Impending Perforation