J Korean Ophthalmol Soc.
2013 Jul;54(7):1109-1113. 10.3341/jkos.2013.54.7.1109.
Primary Orbital MALT Lymphoma Associated with Localized Amyloidosis
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ydkimoph@skku.edu
- KMID: 2217424
- DOI: http://doi.org/10.3341/jkos.2013.54.7.1109
Abstract
- PURPOSE
To report a case of primary orbital MALT lymphoma with localized amyloidosis.
CASE SUMMARY
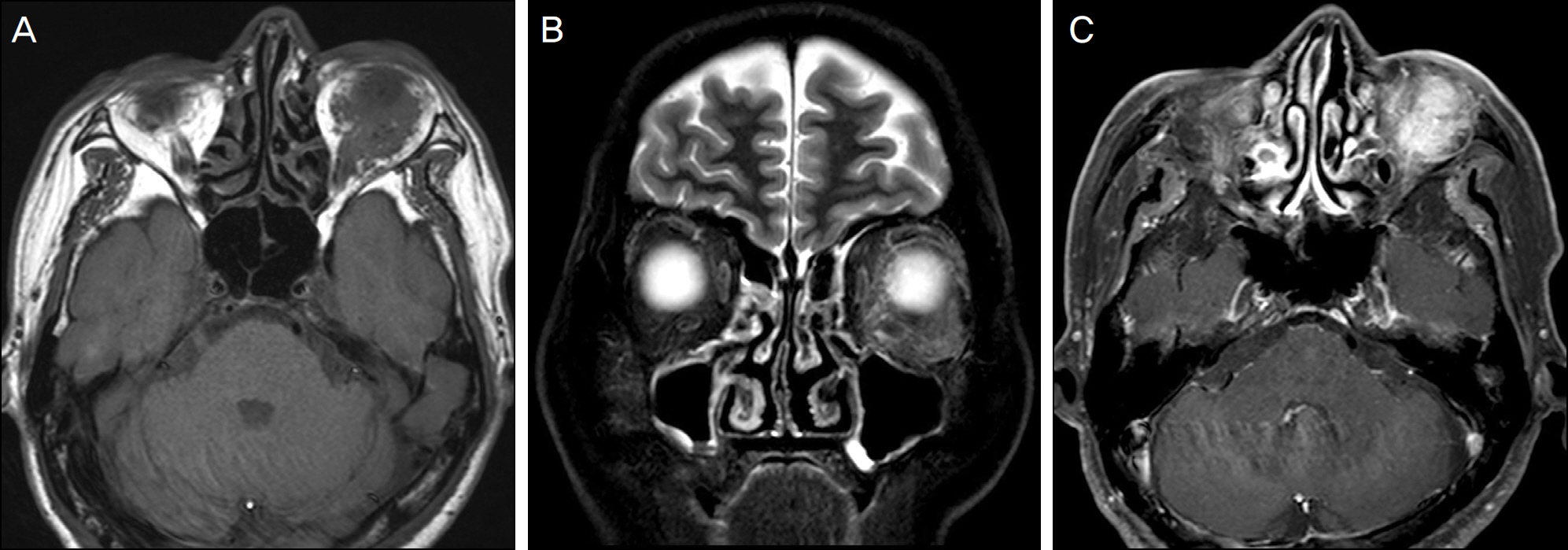
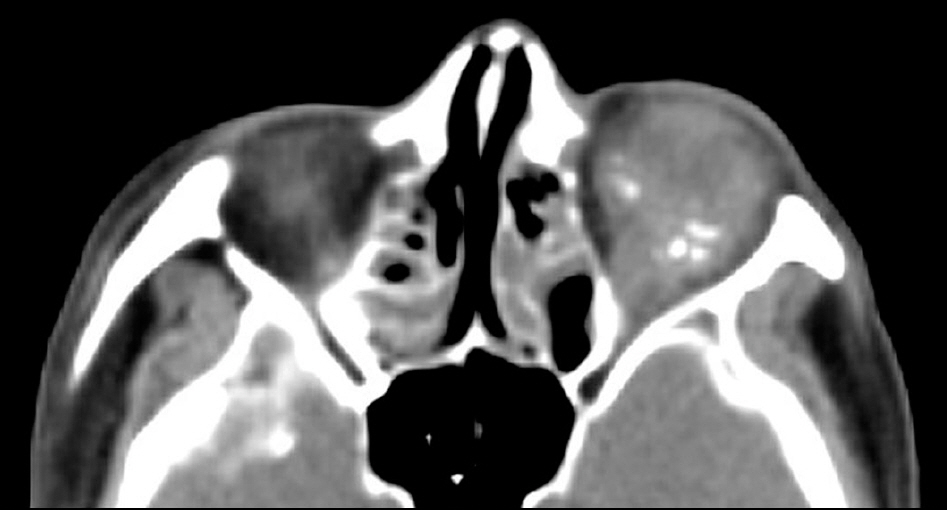
A 61-year-old male visited our clinic with diplopia, which had developed approximately 5 months earlier. Magnetic resonance imaging of the orbit showed an ill-defined well-enhanced mass in the left inferior orbit. Incisional biopsy of the orbital mass was performed. Histopathological examination revealed diffuse deposits of an amorphous, eosinophilic substance in the extracellular matrix and vessels with lymphocytes infiltration. Lymphocytes were positive for the immunohistochemical stain against the CD20 and kappa-light chain antigens. The amorphous material stained positive for kappa-light chain antigen, and Congo red staining showed birefringence.
CONCLUSIONS
We report a rare case of primary orbital MALT lymphoma associated with localized amyloidosis.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Primary Systemic Amyloidosis of the Eyelid: A Case Report
Yeon Soo Kang, Won Choi, Kyung Chul Yoon
J Korean Ophthalmol Soc. 2015;56(7):1117-1121. doi: 10.3341/jkos.2015.56.7.1117.
Reference
-
References
1. Spencer WH. Ophthalmic Pathology, 3rd ed. Philadelphia:: WB Saunders;1985. p. 2672–98.2. Yoon JS, Ma KT, Kim SJ, et al. Prognosis for patients in a Korean population with ocular adnexal lymphoproliferative lesions. Ophthal Plast Reconstr Surg. 2007; 23:94–9.
Article3. Meunier J, Lumbroso-Le Rouic L, Vincent-Salomon A, et al. Ophthalmologic and intraocular non-Hodgkin's lymphoma: a large single centre study of initial characteristics, natural history, and prognostic factors. Hematol Oncol. 2004; 22:143–58.
Article4. Knowles DM 2nd, Jakobiec FA, Rosen M, Howard G. Amyloidosis of the orbit and adnexae. Surv Ophthalmol. 1975; 19:367–84.5. Picken MM. New insights into systemic amyloidosis: the im-portance of diagnosis of specific type. Curr Opin Nephrol Hypertens. 2007; 16:196–203.
Article6. Leibovitch I, Selva D, Goldberg RA, et al. Periocular and orbital amyloidosis: clinical characteristics, management, and outcome. Ophthalmology. 2006; 113:1657–64.7. Murdoch IE, Sullivan TJ, Moseley I, et al. Primary localised amy-loidosis of the orbit. Br J Ophthalmol. 1996; 80:1083–6.
Article8. Goshe JM, Schoenfield L, Emch T, Singh AD. Myeloma-asso-ciated orbital amyloidosis. Orbit. 2010; 29:274–7.
Article9. Dacic S, Colby TV, Yousem SA. Nodular amyloidoma and primary pulmonary lymphoma with amyloid production: a differential di-agnostic problem. Mod Pathol. 2000; 13:934–40.
Article10. Caulet S, Robert I, Bardaxoglou E, et al. Malignant lymphoma of mucosa associated lymphoid tissue: a new etiology of amyloidosis. Pathol Res Pract. 1995; 191:1203–7.
Article11. Goteri G, Ranaldi R, Pileri SA, Bearzi I. Localized amyloidosis and gastrointestinal lymphoma: a rare association. Histopathology. 1998; 32:348–55.
Article12. Wieker K, Röcken C, Koenigsmann M, et al. Pulmonary low-grade MALT-lymphoma associated with localized pulmonary amyloidosis. A case report. Amyloid. 2002; 9:190–3.13. Gupta D, Shidham V, Zemba-Palko V, Keshgegian A. Primary bi-lateral mucosa-associated lymphoid tissue lymphoma of the breast with atypical ductal hyperplasia and localized amyloidosis. A case report and review of the literature. Arch Pathol Lab Med. 2000; 124:1233–6.
Article14. Haas BD, Margo CE. Orbital lymphoma, amyloid, and bone. Ophthalmology. 2007; 114:1237.
Article15. Khaira M, Mutamba A, Meligonis G, et al. The use of radiotherapy for the treatment of localized orbital amyloidosis. Orbit. 2008; 27:432–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Localized Orbital Amyloidosis
- A Case of Laryngeal Mucosa Associated Lymphoid Tissue Lymphoma Mimicking Laryngeal Amyloidosis
- A Newly Developed Gastric MALT Lymphoma after Cure of Jejunal MALT Lymphoma : A Case Report
- Primary localized amyloidosis of the bladder: a case report
- Primary Localized Amyloidosis of Bulbar Conjunctiva and Cornea