J Korean Ophthalmol Soc.
2015 Jan;56(1):39-46. 10.3341/jkos.2015.56.1.39.
Short-Term Outcome of Intravitreal Dexamethasone Implant for Macular Edema Secondary to Branch Retinal Vein Occlusion
- Affiliations
-
- 1Department of Ophthalmology, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea. kjh7997@daum.net
- KMID: 2216152
- DOI: http://doi.org/10.3341/jkos.2015.56.1.39
Abstract
- PURPOSE
To evaluate short-term outcomes of intavitreal dexamethasone implant in macular edema secondary to branch retinal vein occlusion (BRVO).
METHODS
A retrospective review of medical records was performed for 24 patients (24 eyes) who were diagnosed with macular edema secondary to BRVO. The best-corrected visual acuity (BCVA) and central foveal thickness (CFT) were measured before the injection and at 1 and 3 months after the injection. The values measured before and after the treatment were compared. In addition, the association between duration of symptoms and 3-month changes in BCVA was evaluated.
RESULTS
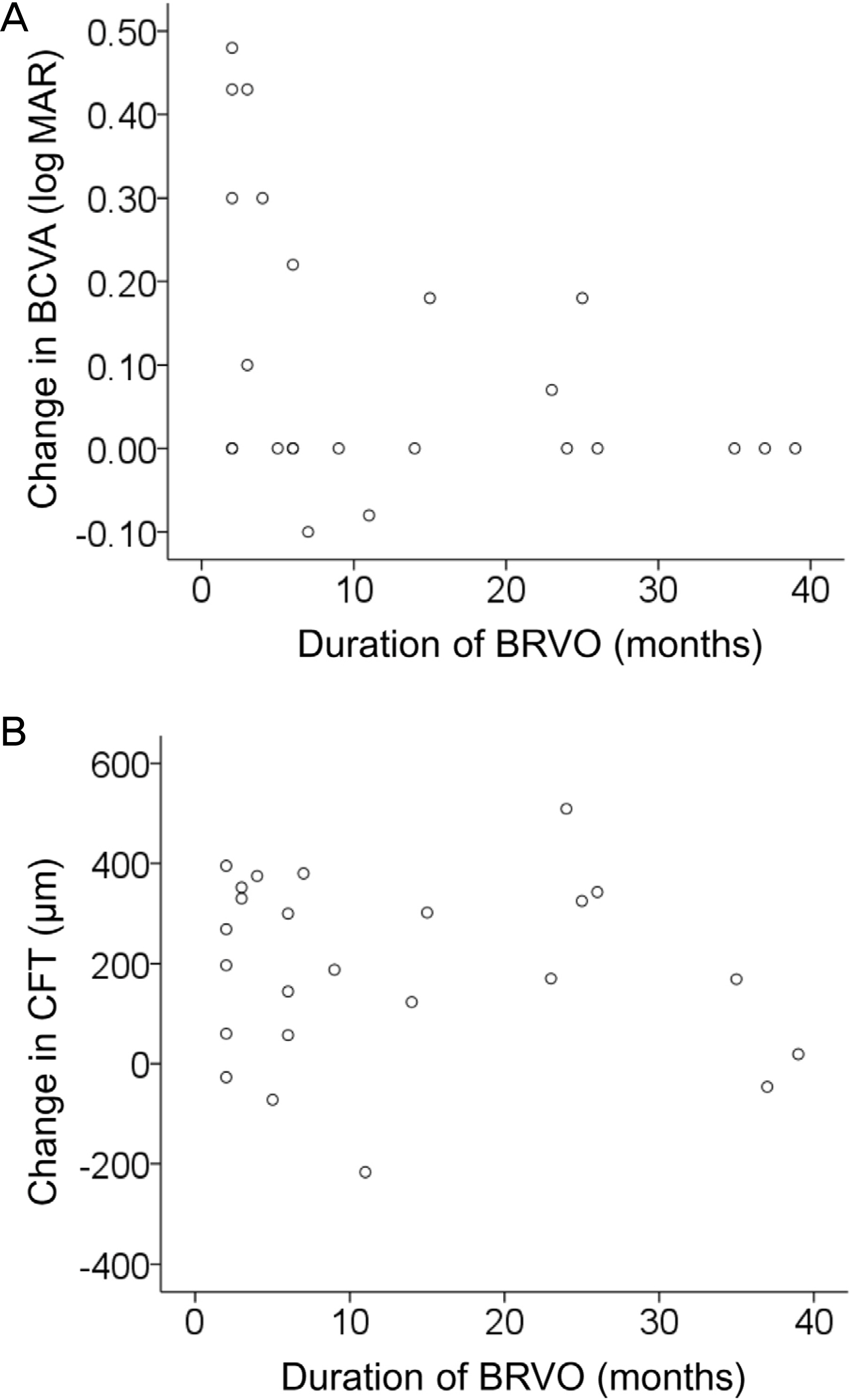
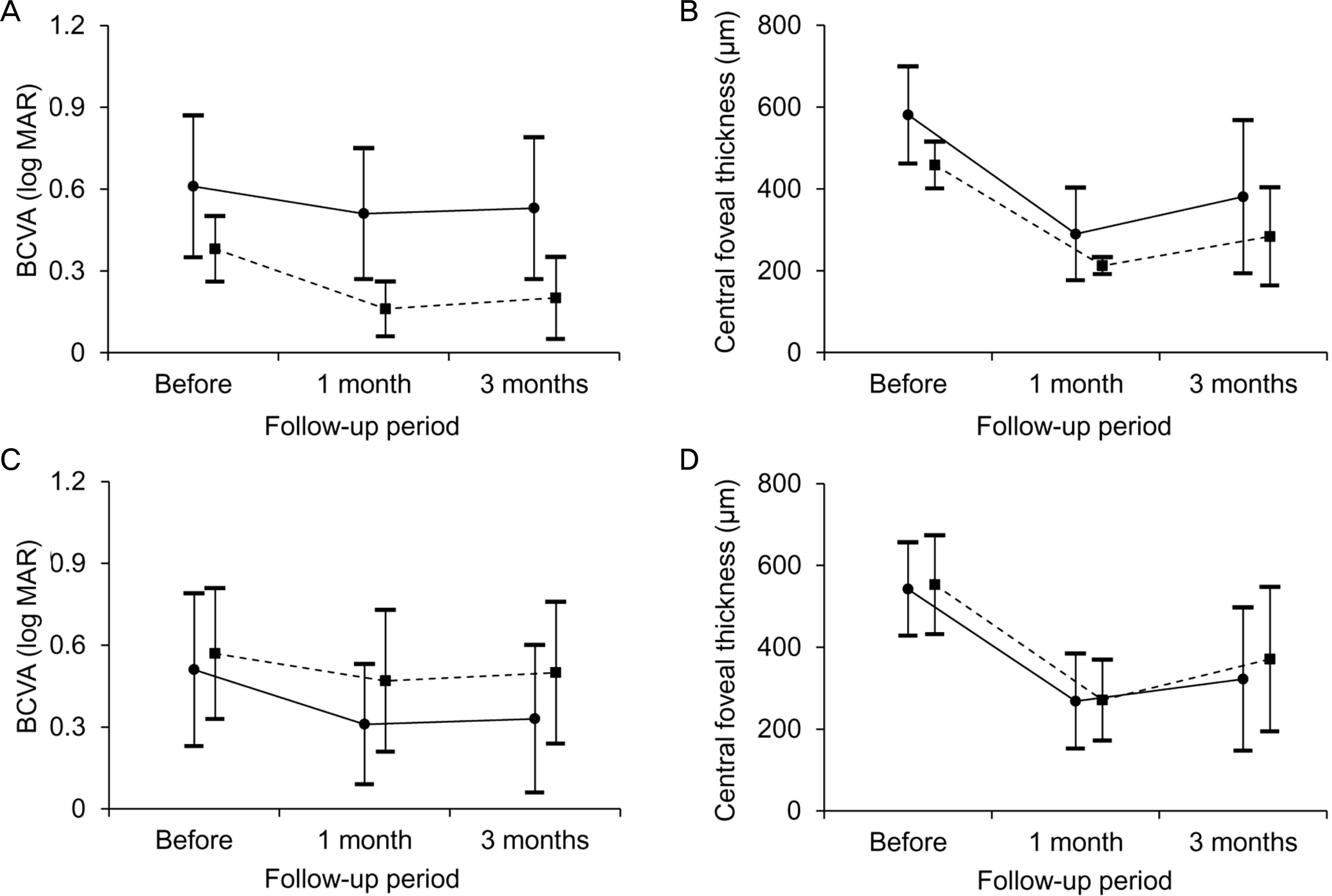
In 24 eyes, the logarithm of minimal angle of resolution BCVA before the injection and 1 and 3 months after the injection was 0.56 +/- 0.25, 0.42 +/- 0.26 and 0.45 +/- 0.27, respectively. The CFT was 550.2 +/- 116.5 microm, 270.3 +/- 101.5 microm, and 356.6 +/- 173.7 microm, respectively. When compared with the baseline values, the BCVA at 3 months was significantly improved (p = 0.018) and the CFT was significantly decreased (p < 0.001). There was a significant negative association between the duration of symptoms and 3-month changes in BCVA (p = 0.032, r = -0.375). Elevated intraocular pressure was observed in 3 eyes (12.5%).
CONCLUSIONS
Intravitreal dexamethasone implant was found effective in treating macular edema secondary to BRVO. However, rebound macular edema and deterioration in visual acuity after 1 month suggest further studies with longer follow-ups are necessary.
MeSH Terms
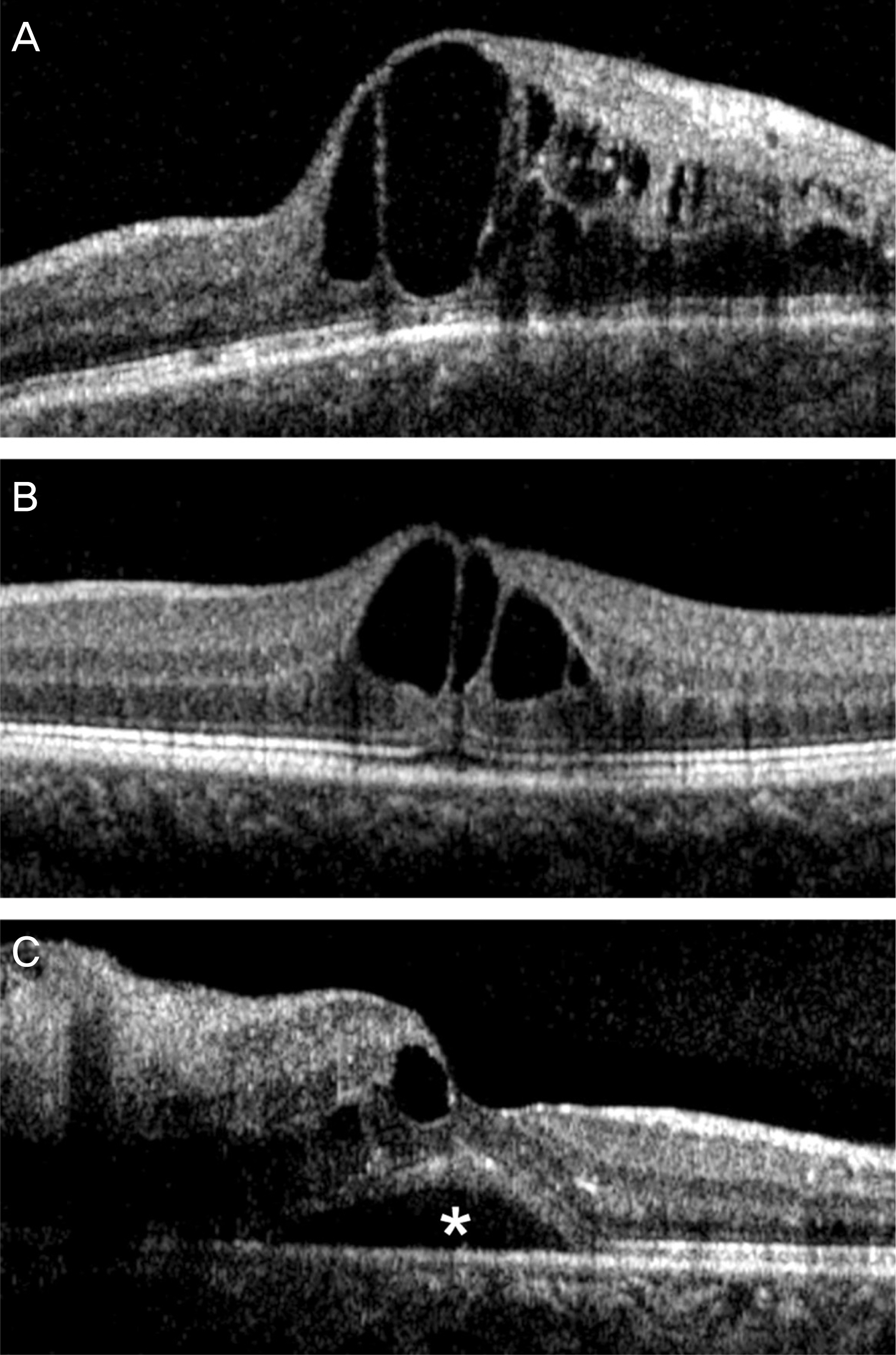
Figure
Reference
-
References
1. Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res. 2005; 24:493–519.
Article2. Rogers SL, McIntosh RL, Lim L. . Natural history of branch retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010; 117:1094–101.e5.
Article3. McIntosh RL, Rogers SL, Lim L. . Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010; 117:1113–23.e15.
Article4. Campochiaro PA, Hafiz G, Shah SM. . Ranibizumab for macular edema due to retinal vein occlusions: implication of VEGF as a critical stimulator. Mol Ther. 2008; 16:791–9.
Article5. Shin HY, Jee DH. The short-term efficacy of intravitreal ranibizu-mab for macular edema in central retinal vein occlusion. J Korean Ophthalmol Soc. 2011; 52:1048–54.
Article6. Lee YS, Kim MS, Yu SY, Kwak HW. Two-year results of intra-vitreal bevacizumab injection in retinal vein occlusion. J Korean Ophthalmol Soc. 2011; 52:1039–47.
Article7. Campochiaro PA, Brown DM, Awh CC. . Sustained benefits from ranibizumab for macular edema following central retinal vein occlusion: twelve-month outcomes of a phase III study. Ophthalmology. 2011; 118:2041–9.
Article8. Brown DM, Campochiaro PA, Bhisitkul RB. . Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology. 2011; 118:1594–602.
Article9. Kuppermann BD, Blumenkranz MS, Haller JA. . Randomized controlled study of an intravitreous dexamethasone drug delivery system in patients with persistent macular edema. Arch Ophthalmol. 2007; 125:309–17.
Article10. Haller JA, Bandello F, Belfort R Jr. . Randomized, sham-con-trolled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010; 117:1134–46.e3.
Article11. Youn SM, Park SJ, Lee HY. . A case of dexamethasone intravitreal implant fragmentation during the injection procedure in central retinal vein occlusion. J Korean Ophthalmol Soc. 2013; 54:982–6.
Article12. Han HC, Bang JW, Yum JH. . A case of acute endophthalmitis following a dexamethasone intravitreal implant. J Korean Ophthalmol Soc. 2013; 54:1939–44.
Article13. Park KH, Rho IH. Short-term visual outcomes according to patterns of macular edema in retinal vein occlusion patients. J Korean Ophthalmol Soc. 2012; 53:1276–84.
Article14. Joshi L, Yaganti S, Gemenetzi M. . Dexamethasone implants in retinal vein occlusion: 12-month clinical effectiveness using repeat injections as-needed. Br J Ophthalmol. 2013; 97:1040–4.
Article15. Matonti F, Meyer F, Guigou S. . Ozurdex in the management of the macular edema following retinal vein occlusion in clinical practice. Acta Ophthalmol. 2013; 91:e584–6.
Article16. Sharareh B, Gallemore R, Taban M. . Recalcitrant macular edema after intravitreal bevacizumab is responsive to an intravitreal dexamethasone implant in retinal vein occlusion. Retina. 2013; 33:1227–31.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Retinal Hemorrhage Following a Dexamethasone Intravitreal Implant
- A Comparison of Three Intravitreal Modalities of Branch Retinal Vein Occlusion Macular Edema
- Intravitreal Dexamethasone Implant for Macular Edema in Branch Retinal Vein Occlusion According to Previous Responses to Bevacizumab
- A Case of Dexamethasone Intravitreal Implant Fragmentation During the Injection Procedure in Central Retinal Vein Occlusion
- A Case of Acute Endophthalmitis Following a Dexamethasone Intravitreal Implant