J Korean Ophthalmol Soc.
2012 Sep;53(9):1330-1333. 10.3341/jkos.2012.53.9.1330.
A Case of Conjunctival Hemorrhagic Lymphangiectasia
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University College of Medicine, Seoul, Korea. schcornea@schmc.ac.kr
- KMID: 2216088
- DOI: http://doi.org/10.3341/jkos.2012.53.9.1330
Abstract
- PURPOSE
To report a case of hemorrhagic lymphangiectasia treated with surgical excision and confirmed by pathologic examination.
CASE SUMMARY
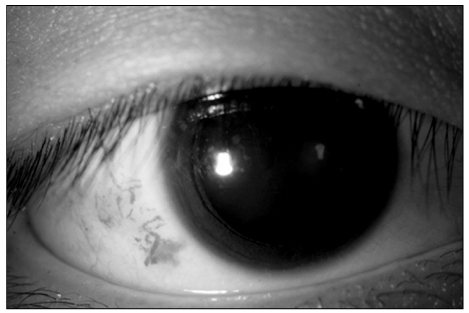
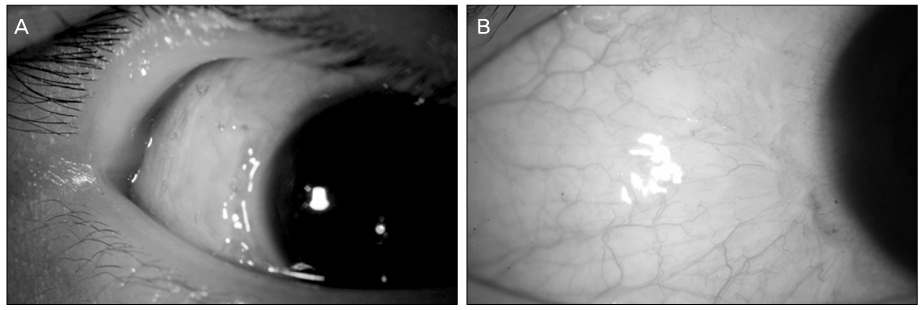
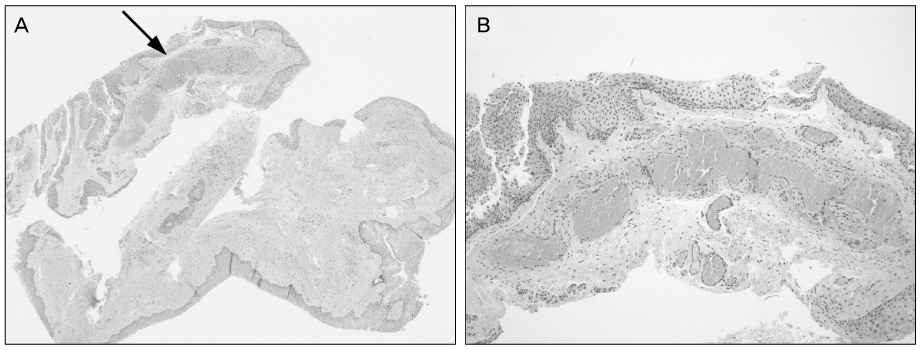
A 21-year-old man presented with spontaneous hyperemia of his right eye of 1 week duration. The patient had a history of tuberculous retinal vasculitis and uveitis 1 year prior, but there was no active lesion during regular follow-up. There was no history of trauma, visual disturbance, diplopia, ocular pain, or any sign of systemic disease. Slit lamp examination showed tortuous dilatation of blood-filled lymphatic vessels on temporal conjunctiva of the right eye. The lesion did not change during the 4 weeks of follow-up and local excision biopsy was made for final diagnosis and treatment. Pathologic examinations revealed thin-walled lymphatic vessels with localized dilatation which contained blood in the lumen consistent with hemorrhagic lymphangiectasia. There was no sign of recurrence until 2 months after the operation.
CONCLUSIONS
Hemorrhagic lymphangiectasia should be considered in patients with recurrent or longstanding localized tortuous subconjunctival hemorrhage.
MeSH Terms
Figure
Cited by 1 articles
-
360° Circumferential Hemorrhagic Lymphangiectasia of the Conjunctivae
Su Jin Park, Mijung Chi
J Korean Ophthalmol Soc. 2020;61(3):298-302. doi: 10.3341/jkos.2020.61.3.298.
Reference
-
1. Leber T. Lymphangiectasia haemorrhagica conjunctivae. Graefes Arch Ophthalmol. 1880. 26:197–201.2. Chelsky MP, Magnus DE. Conjunctival hemorrhagic lymphangiectasis. J Am Optom Assoc. 1988. 59:676–678.3. Scott KR, Tse DT, Kronish JW. Hemorrhagic lymphangiectasia of the conjunctiva. Arch Ophthalmol. 1991. 109:286–287.4. Jampol LM, Nagpal KC. Hemorrhagic lymphangiectasia of the conjunctiva. Am J Ophthalmol. 1978. 85:419–420.5. Duke-Elder S, Leigh AG. System of Ophthalmology. Vol. 8. Diseases of the Outer Eye. 1965. St. Louis: CV Mosby;40–42. 1198–1207.6. Lee SW, Lee SE, Jin KH. Conjunctival inclusion cysts in long-standing chronic vernal keratoconjunctivitis. Korean J Ophthalmol. 2007. 21:251–254.7. Singh G, Rajaraman R, Raghavan A, Palanisamy M. Bilateral conjunctival retention cysts in the aftermath of Stevens-Johnson syndrome. Indian J Ophthalmol. 2008. 56:70–72.8. Krachmer JH, Mannis MJ, Holland EJ. Cornea. 2011. Vol. 1:3rd ed. St. Louis: Mosby;488–489.9. Soong HK, Pollock DA. Hereditary hemorrhagic telangiectasia diagnosed by the ophthalmologist. Cornea. 2000. 19:849–850.10. Wasfy IA. Lymphangiectasia haemorrhagica conjunctivae: report of three cases with a note on successful treatment with cryosurgery in one case. Bull Ophthalmol Soc Egypt. 1975. 68:37–44.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Surgery for Conjunctival Lymphangiectasia Using a High-frequency Radio Wave Electrosurgical Unit
- Idiopathic Intestinal Lymphangiectasia
- 360° Circumferential Hemorrhagic Lymphangiectasia of the Conjunctivae
- The Update of Treatment for Primary Intestinal Lymphangiectasia
- A Case of Primary Intestinal Lymphangiectasia Diagnosed by Double Balloon Enteroscopy