J Korean Ophthalmol Soc.
2011 Jun;52(6):726-733. 10.3341/jkos.2011.52.6.726.
Postoperative Visual Field Outcomes in Patients Showing Visual Field Defects due to Pituitary Adenoma
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University Bucheon Hospital, College of Medicine, Soonchunhyang University, Bucheon, Korea. genophilus@hanmail.net
- 2Department of Neurosurgery, Soonchunhyang University Bucheon Hospital, College of Medicine, Soonchunhyang University, Bucheon, Korea.
- KMID: 2214646
- DOI: http://doi.org/10.3341/jkos.2011.52.6.726
Abstract
- PURPOSE
To evaluate visual field (VF) changes in patients with pituitary adenoma after surgical treatment.
METHODS
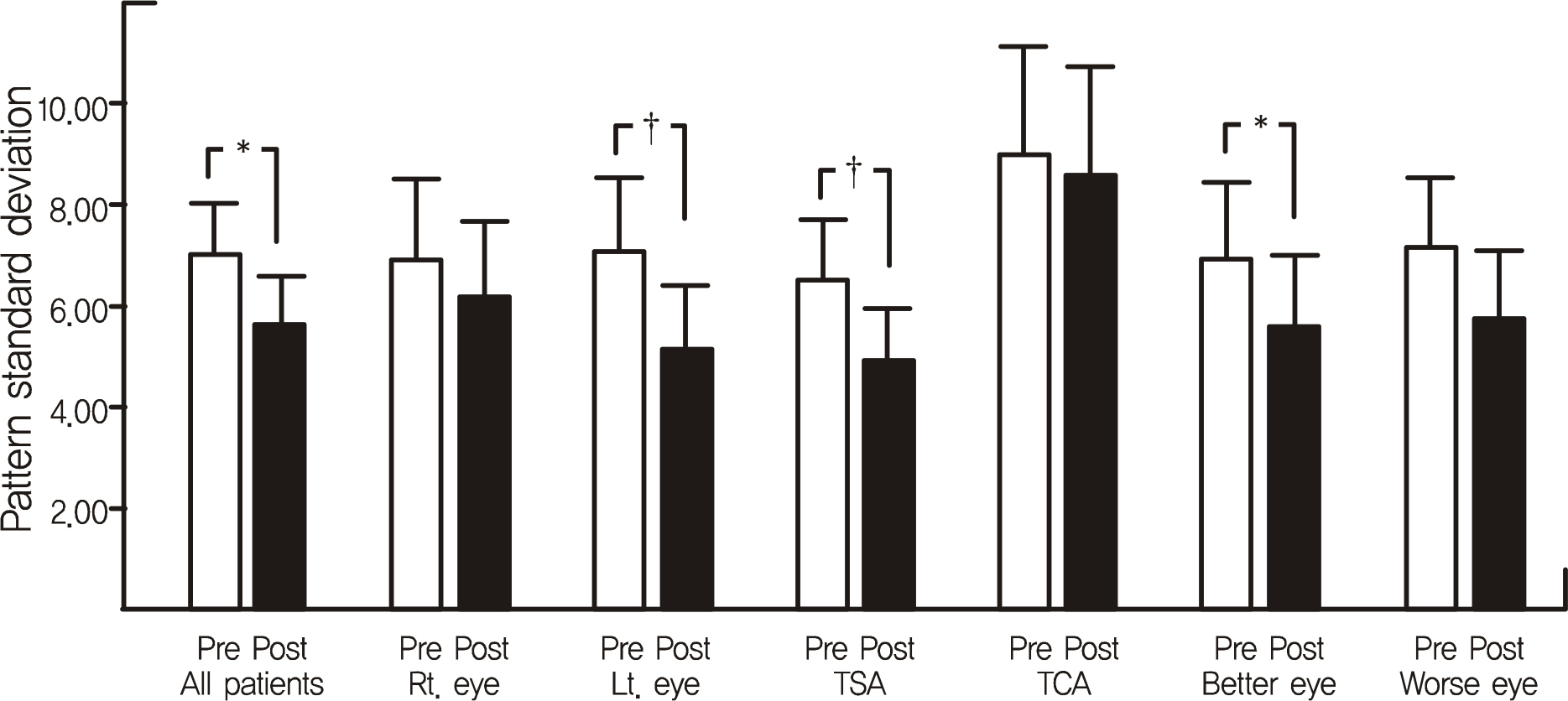
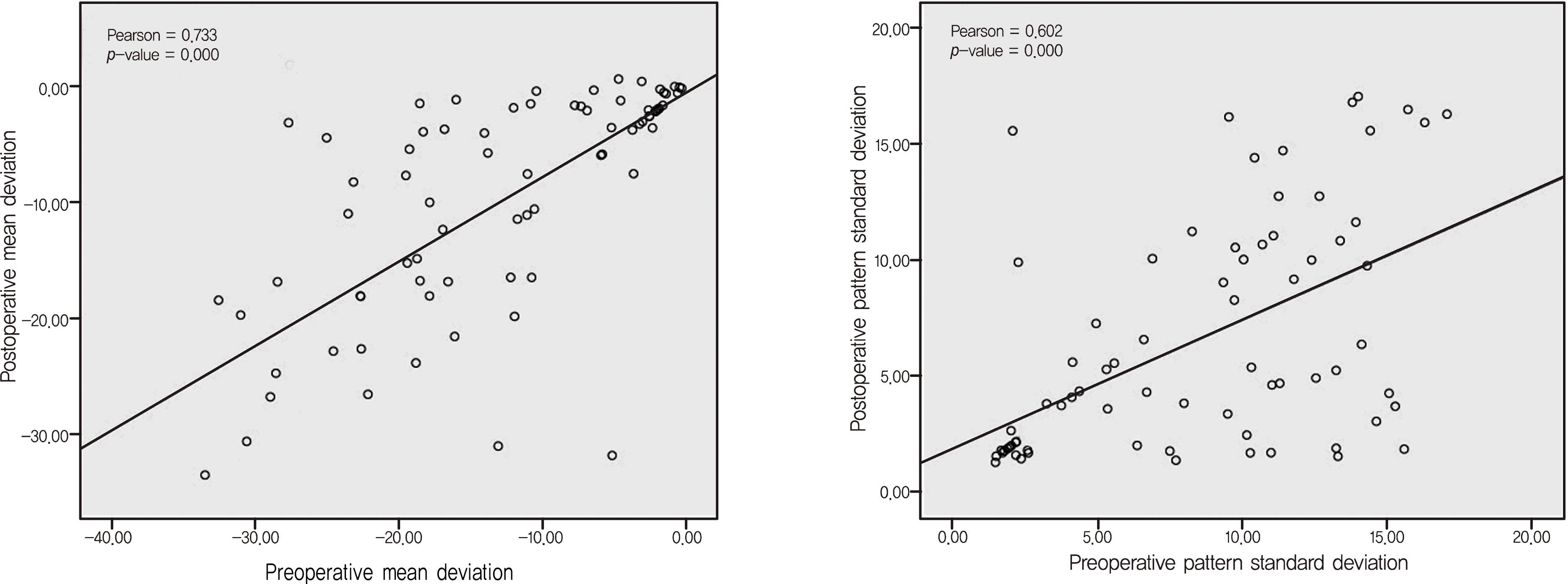
The present study retrospectively evaluated 96 eyes of 48 patients with pituitary adenoma who received surgical tumor removal between July 2001 and February 2010. Preoperative and postoperative clinical data including age, tumor volume, logMAR BCVA, surgical technique (transsphenoidal surgery and transcranial surgery), static perimetry scores (mean deviation [MD], pattern standard deviation [PSD], and visual field defect [VFD] scores) were reviewed.
RESULTS
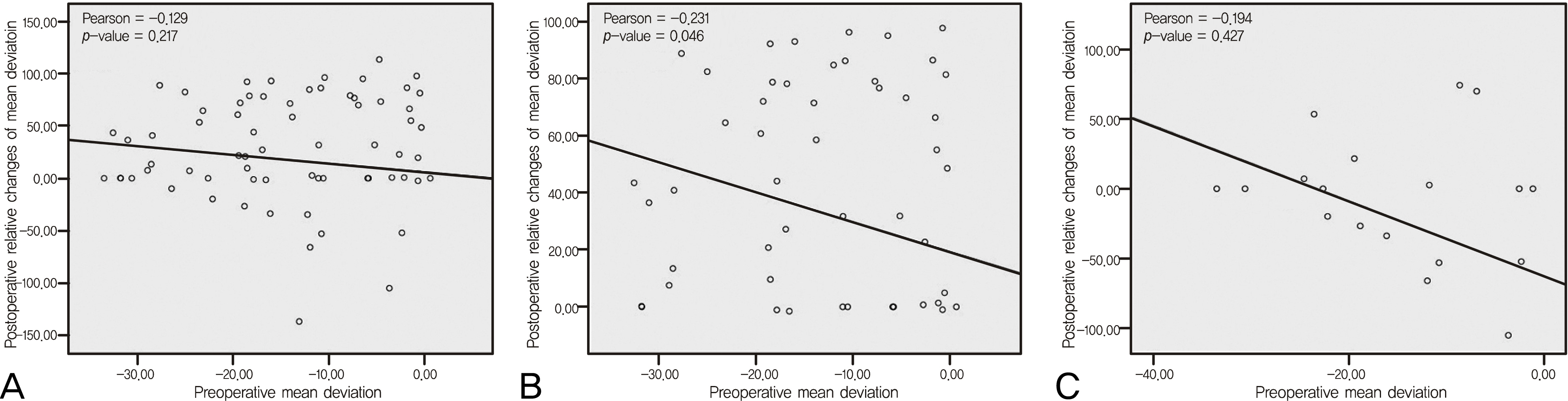
The MD (15.79%, p = 0.001) and PSD (3.98%, p = 0.003) improved postoperatively (mean postoperative follow-up period 1.85 months). Transsphenoidal surgery for tumor removal showed significant MD (26.99%, p = 0.000) and PSD (12.92%, p = 0.003) improvements. A multivariate regression analysis of the transsphenoidal surgery patient group revealed that the preoperative MD was related to the postoperative MD (Pearson = 0.762, p = 0.000), but negatively correlated to the amount of postoperative improvement in MD score (Pearson = -0.231, p = 0.046). Transcranial surgery did not significantly improve the MD (p = 0.419), PSD (p = 0.562), VFD score (p = 0.135), or logMAR BCVA (p = 0.708).
CONCLUSIONS
Visual filed defects in patients with pituitary adenoma improved after neurosurgical treatment. Better postoperative visual field outcomes were achieved in patients who had smaller preoperative visual field defects. Transsphenoidal surgery significantly improved the visual field defects and visual acuity in patients with non-functioning pituitary adenoma, compared to the transcranial surgery patients.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Kerrison JB, Lynn MJ, Baer CA, et al. Stages of improvement in visual fields after pituitary tumor resection. Am J Ophthalmol. 2000; 130:813–20.
Article2. Laws ER Jr, Trautmann JC, Hollenhorst RW Jr. Transsphenoidal decompression of the optic nerve and chiasm. Visual results in 62 patients. J Neurosurg. 1977; 46:717–22.3. Powell M. Recovery of vision following transsphenoidal surgery for pituitary adenomas. Br J Neurosurg. 1995; 9:367–73.
Article4. Svien HJ, Love JG, Kennedy WC, et al. Status of vision following surgical treatment for pituitary chromophobe adenoma. J Neurosurg. 1965; 22:47–52.
Article5. Ciric I, Mikhael M, Stafford T, et al. Transsphenoidal microsurgery of pituitary macroadenomas with long-term follow-up results. J Neurosurg. 1983; 59:395–401.
Article6. Findlay G, McFadzean RM, Teasdale G. Recovery of vision following treatment of pituitary tumours: application of a new system of visual assessment. Trans Ophthalmol Soc U K. 1983; 103:212–6.7. Lennerstrand G. Visual recovery after treatment for pituitary adenoma. Acta Ophthalmol. 1983; 61:1104–17.
Article8. Gnanalingham KK, Bhattacharjee S, Pennington R, et al. The time course of visual field recovery following transphenoidal surgery for pituitary adenomas: predictive factors for a good outcome. J Neurol Neurosurg Psychiatry. 2005; 76:415–9.
Article9. Cohen AR, Cooper PR, Kupersmith MJ, et al. Visual recovery after transsphenoidal removal of pituitary adenomas. Neurosurgery. 1985; 17:446–52.
Article10. Ogden TE. Nerve fiber layer of the primate retina: thickness and glial content. Vision Res. 1983; 23:581–7.
Article11. Blamires TL, Reeves BC. Vision defects in patients with peri-chiasmal lesions. Optom Vis Sci. 1996; 73:572–8.
Article12. Hirai T, Ito Y, Arai M, et al. Loss of stereopsis with optic chiasmal lesions and stereoscopic tests as a differential test. Ophthalmology. 2002; 109:1692–702.
Article13. Symon L, Jakubowski J. Transcranial management of pituitary tumours with suprasellar extension. J Neurol Neurosurg Psychiatry. 1979; 42:123–33.
Article14. Wang H, Sun W, Fu Z, et al. The pattern of visual impairment in patients with pituitary adenoma. J Int Med Res. 2008; 36:1064–9.
Article15. Thomas R, Shenoy K, Seshadri MS, et al. Visual field defects in non-functioning pituitary adenomas. Indian J Ophthalmol. 2002; 50:127–30.16. Feinsod M, Selhorst JB, Hoyt WF, Wilson CB. Monitoring optic nerve function during craniotomy. J Neurosurg. 1976; 44:29–31.
Article17. Smith EJ, Blakemore WF, McDonald WI. Central remyelination restores secure conduction. Nature. 1979; 280:395–6.
Article18. Seddon HJ, Medawar PB, Smith H. Rate of regeneration of peripheral nerves in man. J Physiol. 1943; 102:191–215.
Article19. Seddon HJ. A classification of nerve injuries. Br Med J. 1942; 2:237–9.
Article20. Donoff RB. Nerve regeneration: basic and applied aspects. Crit Rev Oral Biol Med. 1995; 6:18–24.
Article21. Couldwell WT. Transsphenoidal and transcranial surgery for pituitary adenomas. J Neurooncol. 2004; 69:237–56.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Location and Size of Pituitary Adenoma and Visual Field Change
- Postoperative Visual Results on Sellar and Parasellar Tumors
- Factors Influencing Visual Field Recovery after Transsphenoidal Resection of a Pituitary Adenoma
- Visual Field Defects and Disc Findings in Glaucoma
- Analysis of Factors Related of Location of Initial Visual Field Defect in Normal Tension Glaucoma