J Korean Ophthalmol Soc.
2011 May;52(5):519-523. 10.3341/jkos.2011.52.5.519.
Learning Curve for Endonasal Dacryocystorhinostomy
- Affiliations
-
- 1Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. sjh@med.yu.ac.kr
- KMID: 2214569
- DOI: http://doi.org/10.3341/jkos.2011.52.5.519
Abstract
- PURPOSE
To determine the learning curve of dacryocystorhinostomy (DCR) performed by a single oculoplastic surgeon after one year of fellowship training.
METHODS
This retrospective review study comprised nasolacrimal duct obstruction patients that underwent endonasal DCR at our hospital between February 2006 and February 2008. The patients that completed at least six months of follow-up were included in the analysis. Exclusion criteria were patients less than 20 years of age and NLD obstructions due to malignancy or canalicular obstructions. Success was defined as duct patency on syringing at the final follow-up and no complaints of epiphora.
RESULTS
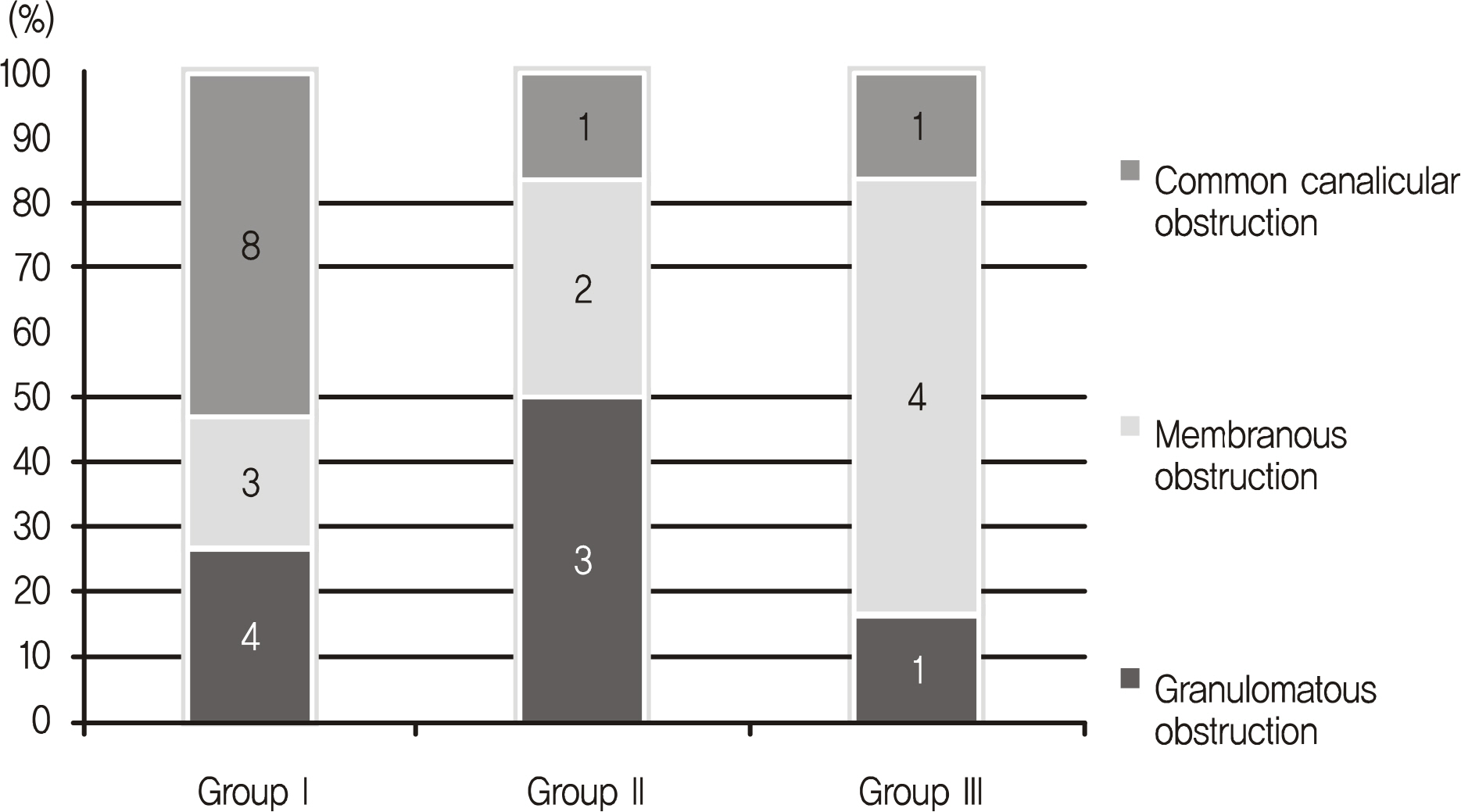
Out of 161 eyes, the overall surgical success rate was 83.2% (134/161 eyes) and the mean postoperative follow-up period was 6.5 months (6-18 months). Success rates gradually increased as follows: 71.2% (37/52 eyes) for the first group, 88.7% (47/53 eyes) for the second group, and 89.3% (50/56 eyes) for the third group (second and third group compared to first group, p = 0.025, p = 0.017, respectively).
CONCLUSIONS
To ensure high DCR success rates, the novice surgeon should perform at least 50 surgeries.
MeSH Terms
Figure
Cited by 2 articles
-
Analysis of the Results Endonasal Dacryocystorhinostomy Related to Nasal Cavity State
Seung Kook Baek, Myung Sook Ha
J Korean Ophthalmol Soc. 2014;55(5):633-639. doi: 10.3341/jkos.2014.55.5.633.Learning Curve for Strabismus Surgery
Jang Hun Lee, Sang Beom Han, Seung Jun Lee, Moo Sang Kim
J Korean Ophthalmol Soc. 2015;56(7):1111-1116. doi: 10.3341/jkos.2015.56.7.1111.
Reference
-
References
1. Caldwell GW. Two new operations for obstructions of the nasal duct with preservation of the canaliculi. Am J Ophthalmol. 1893; 10:189.2. Toti A. Nuovo metodo conservatore di cura radiacalle delle sup-purazione cronicle del sacco lacrimale (dacriocistorinostomia). Clin Moderna. 1904; 10:385–9.3. Whittet HB, Shun-Shin GA, Awdry P. Functional endoscopic transnasal dacryocystorhinostomy. Eye. 1993; 7:545–9.
Article4. Kao SC, Liao CL, Tseng JH, et al. Dacryocystorhinostomy with intraoperative mitomycin C. Ophthalmology. 1997; 104:86–91.
Article5. Zilelioğ lu G, Uğ urbaş SH, Anadolu Y, et al. Adjunctive use of mitomycin C on endoscopic lacrimal surgery. Br J Ophthalmol. 1998; 82:63–6.6. Lee SH, Chung WS. Long term surgical efficacy of endonasal dacryo cys torhinostomy. J Korean Ophthalmol Soc. 2000; 41:307–13.7. Ibrahim HA, Batterbury M, Banhegyi G, McGalliard J. Endonasal laser dacryocystorhinostomy and external dacryocystorhinostomy outcome profile in a general ophthalmic service unit: a comparative retrospective study. Ophthalmic Surg Lasers. 2001; 32:220–7.
Article8. Malhotra R, Wright M, Olver JM. A consideration of the time taken to do dacryocystorhinostomy (DCR) surgery. Eye. 2003; 17:691–6.
Article9. Tsirbas A, Davis G, Wormald PJ. Mechanical endonasal dacryocystorhinostomy versus external dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2004; 20:50–6.
Article10. Woog JJ, Kennedy RH, Custer PL, et al. Endonasal dacryocystorhinostomy: a report by the American Academy of Ophthalmology. Ophthalmology. 2001; 108:2369–77.11. Tsirbas A, Wormald PJ. Endonasal dacryocystorhinostomy with mucosal flaps. Am J Ophthalmol. 2003; 135:76–83.
Article12. Martin KR, Burton RL. The phacoemulsification learning curve: per-operative complications in the first 3000 cases of an experienced surgeon. Eye. 2000; 14:190–5.
Article13. Tayanithi P, Pungpapong K, Siramput P. Vitreous loss during phacoemulsification learning curve performed by third-year residents. J Med Assoc Thai. 2005; 88:S89–93.14. Randleman JB, Wolfe JD, Woodward M, et al. The resident surgeon phacoemulsification learning curve. Arch Ophthalmol. 2007; 125:1215–9.
Article15. Rice DH. Endoscopic intranasal dacryocystorhinostomy results in four patients. Arch Otolaryngol Head Neck Surg. 1990; 116:1061.
Article16. Yoon JH, Kim KS, Jung DH, et al. Fontanelle and uncinate process in the lateral wall of the human nasal cavity. Laryngoscope. 2000; 110:281–5.
Article17. Mannor GE, Millman AL. The prognostic value of preoperative dacryocystography in endoscopic intranasal dacryocystorhinostomy. Am J Ophthalmol. 1992; 113:134–7.
Article18. Dolman PJ. Comparison of external dacryocystorhinostomy with nonlaser endonasal dacryocystorhinostomy. Ophthalmology. 2003; 110:78–84.
Article19. Kwon SW, Baek SH. Clinical evaluation of endoscopic endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2004; 45:1403–8.20. Hartikainen J, Antila J, Varpula M, et al. Prospective randomized comparison of endonasal endoscopic dacryocystorhinostomy and external dacryocystorhinostomy. Laryngoscope. 1998; 108:1861–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Learning Curve for Endoscopic Endonasal Dacryocystorhinostomy
- Success Rate of Endonasal Dacryocystorhinostomy Based on the Location of the Lacrimal Sac
- Endonasal Dacryocystorhinostomy
- Clinical Effecd of Endonasal Lacrimal Surgery
- The Effect of Nasal Cavity Abnormality Related to Surgical Success Rate of Endonasal Dacryocystorhinostomy