J Korean Ophthalmol Soc.
2016 Mar;57(3):369-379. 10.3341/jkos.2016.57.3.369.
Intraocular Lens Power Calculations Using Dual Scheimpflug Analyzer
- Affiliations
-
- 1Department of Ophthalmology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. schinn@hanmail.net
- 2Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 2213237
- DOI: http://doi.org/10.3341/jkos.2016.57.3.369
Abstract
- PURPOSE
To investigate the accuracy of intraocular lens power calculations using simulated keratometry (simK) of dual Scheimpflug analyzer and 5 types of formulas in cataract patients.
METHODS
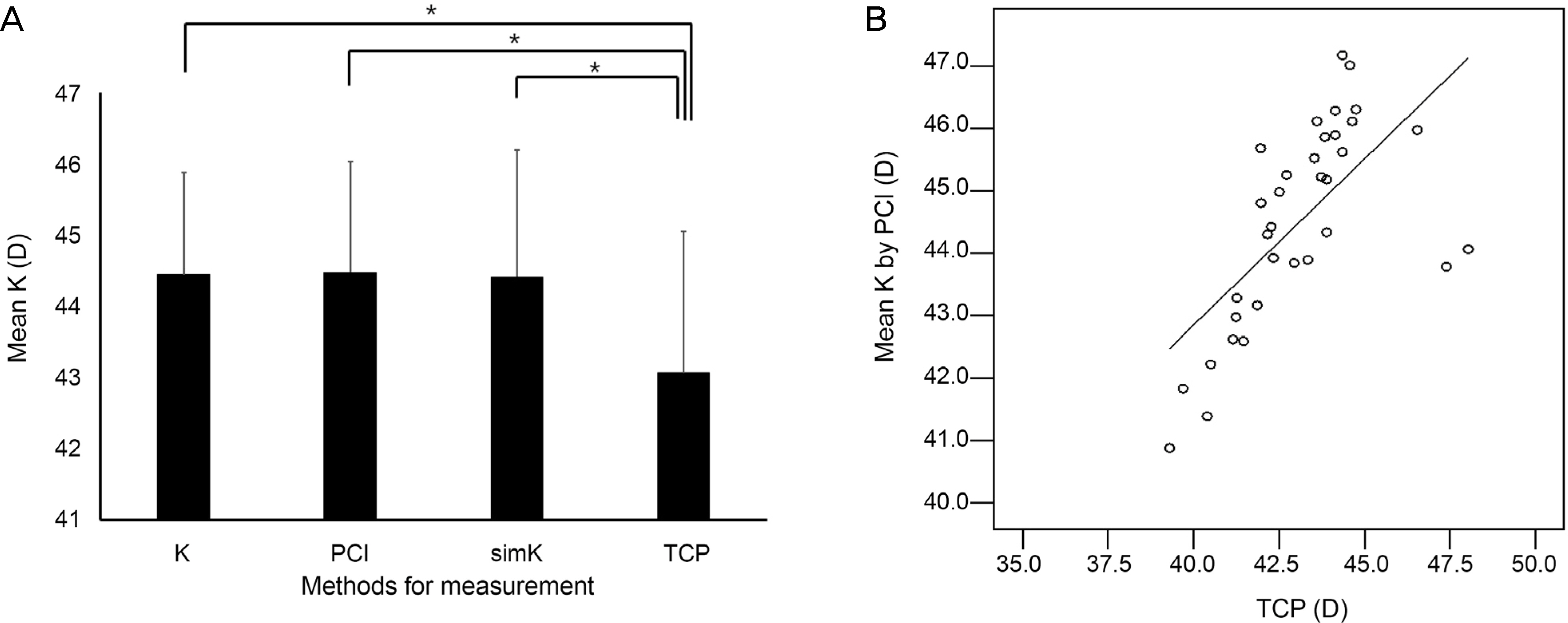
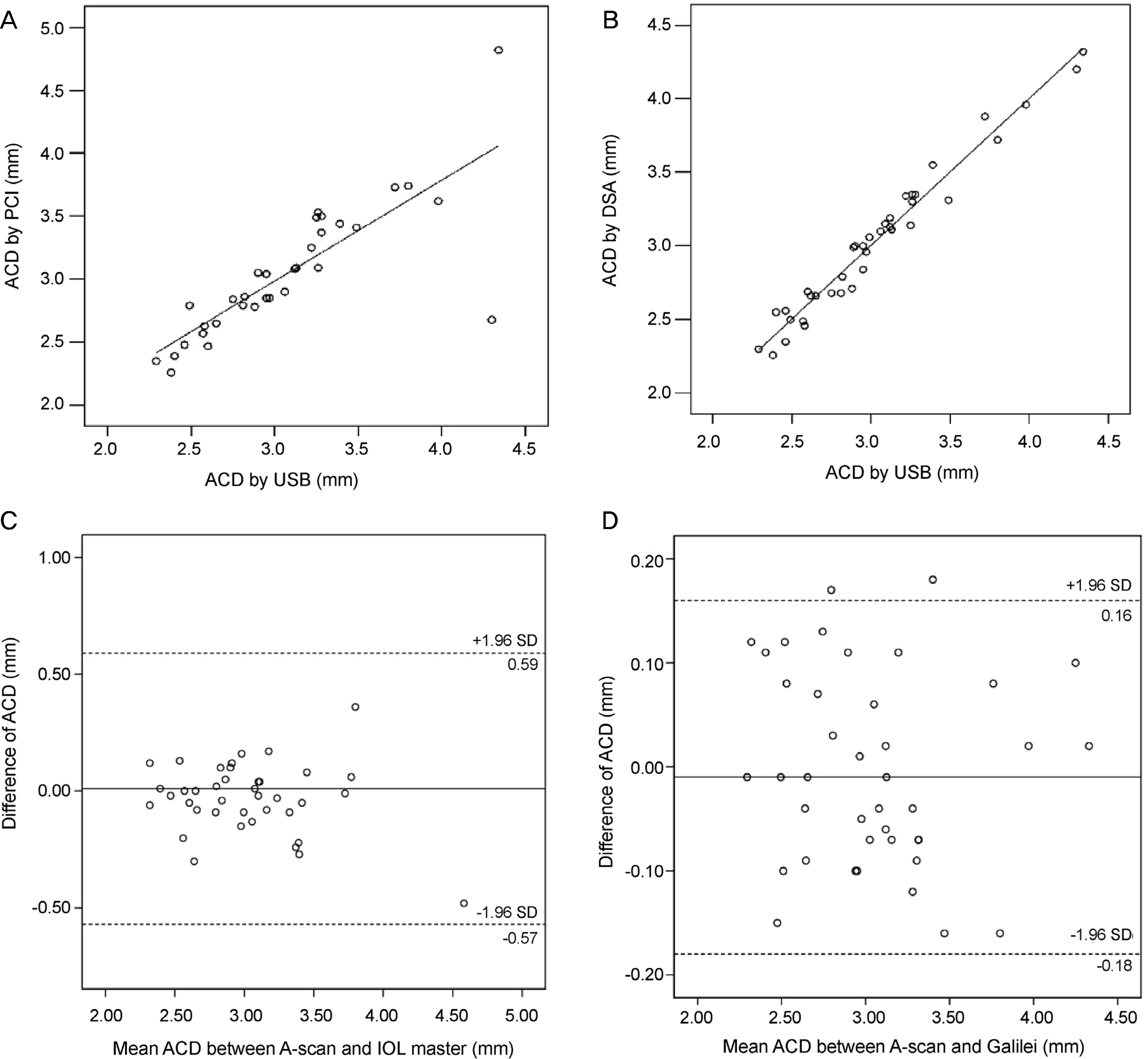
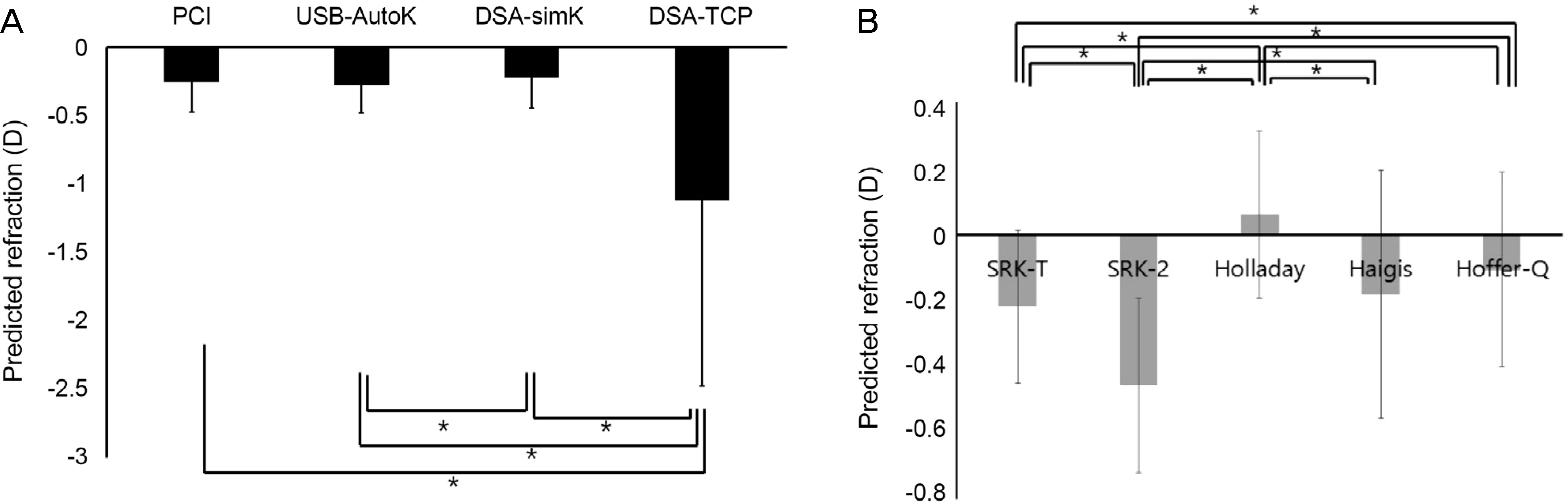
The keratometry (K), axial length (AXL) and anterior chamber depth (ACD) were measured using ultrasound biometry (USB) combined with auto-keratometry (Auto-K), parital coherence interferometry (PCI; IOL master®) and dual Scheimpflug analyzer (DSA; Galilei®) in 39 eyes of 39 patients. Predicted refraction was calculated using Auto-K, mean K of PCI, and simK and total corneal power (TCP) of DSA in the Sanders-Retzlaff-Kraff (SRK-T) formula. The SRK-II, SRK-T, Holladay II, Haigis, and Hoffer-Q formula were used to calculate predicted refraction with the simK of DSA and AXL of USB. Manifest refraction, mean numerical error (MNE) and mean absolute error were evaluated 1, 3 and 6 months after cataract surgery.
RESULTS
TCP of DSA was lower compared with other keratometric values (p < 0.05). The MNE was not different among Auto-K, mean K and simK. The MNE using TCP was larger compared with Auto-K, mean K and simK at 1 month after surgery (p < 0.05). There was a difference in MNE between simK and TCP of DSA at 6 months after surgery (p < 0.05). The MNE of SRK-T formula was the smallest in the intraocular lens (IOL) power calculation using the simK of DSA.
CONCLUSIONS
We suggest using IOL power calculations with simK of DSA and SRK-T formula rather than TCP of DSA in cataract patients with normal corneas.
MeSH Terms
Figure
Reference
-
References
1. Wang JK, Hu CY, Chang SW. Intraocular lens power calculation using the IOLMaster and various formulas in eyes with long axial length. J Cataract Refract Surg. 2008; 34:262–7.
Article2. Preussner PR, Olsen T, Hoffmann P, Findl O. Intraocular lens calculation accuracy limits in normal eyes. J Cataract Refract Surg. 2008; 34:802–8.3. Drexler W, Findl O, Menapace R, et al. Partial coherence interferometry: a novel approach to biometry in cataract surgery. Am J Ophthalmol. 1998; 126:524–34.
Article4. Olsen T. Sources of error in intraocular lens power calculation. J Cataract Refract Surg. 1992; 18:125–9.
Article5. Lam AK, Chan R, Pang PC. The repeatability and accuracy of axial length and anterior chamber depth measurements from the IOLMaster. Ophthalmic Physiol Opt. 2001; 21:477–83.6. Findl O, Drexler W, Menapace R, et al. High precision biometry of pseudophakic eyes using partial coherence interferometry. J Cataract Refract Surg. 1998; 24:1087–93.
Article7. Haigis W, Lege B, Miller N, Schneider B. Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol. 2000; 238:765–73.
Article8. Holladay JT. Standardizing constants for ultrasonic biometry, keratometry, and intraocular lens power calculations. J Cataract Refract Surg. 1997; 23:1356–70.
Article9. Saad E, Shammas MC, Shammas HJ. Scheimpflug corneal power measurements for intraocular lens power calculation in cataract surgery. Am J Ophthalmol. 2013; 156:460–7.e2.
Article10. Savini G, Barboni P, Carbonelli M, Hoffer KJ. Comparison of methods to measure cornealpower for intraocular lens power calculation using a rotating Scheimpflug camera. J Cataract Refract Surg. 2013; 39:598–604.11. Saiki M, Negishi K, Kato N, et al. Ray tracing software for intraocular lens power calculation after corneal excimer laser surgery. Jpn J Ophthalmol. 2014; 58:276–81.
Article12. Savini G, Barboni P, Carbonelli M, Hoffer KJ. Accuracy of Scheimpflug corneal power measurements for intraocular lens power calculation. J Cataract Refract Surg. 2009; 35:1193–7.
Article13. Minami K, Kataoka Y, Matsunaga J, et al. Ray-tracing intraocular lens power calculation using anterior segment optical coherence tomography measurements. J Cataract Refract Surg. 2012; 38:1758–63.
Article14. Shammas HJ, Hoffer KJ, Shammas MC. Scheimpflug photography keratometry readings for routine intraocular lens power calculation. J Cataract Refract Surg. 2009; 35:330–4.
Article15. Savini G, Barboni P, Carbonelli M, Hoffer KJ. Accuracy of a dual Scheimpflug analyzer and a corneal topography system for intraocular lens power calculation in unoperated eyes. J Cataract Refract Surg. 2011; 37:72–6.
Article16. Shirayama M, Wang L, Koch DD, Weikert MP. Comparison of accuracy of intraocular lens calculations using automated keratometry, a Placido-based corneal topographer, and a combined Placido-based and dual Scheimpflug corneal topographer. Cornea. 2010; 29:1136–8.17. Zaldivar R, Shultz MC, Davidorf JM, Holladay JT. Intraocular lens power calculations in patients with extreme myopia. J Cataract Refract Surg. 2000; 26:668–74.
Article18. Findl O. Biometry and intraocular lens power calculation. Curr Opin Ophthalmol. 2005; 16:61–4.
Article19. Rose LT, Moshegov CN. Comparison of the Zeiss IOLMaster and applanation A-scan ultrasound: biometry for intraocular lens calculation. Clin Experiment Ophthalmol. 2003; 31:121–4.
Article20. Németh J, Fekete O, Pesztenlehrer N. Optical and ultrasound measurement of axial length and anterior chamber depth for intraocular lens power calculation. J Cataract Refract Surg. 2003; 29:85–8.
Article21. Utine CA, Altin F, Cakir H, Perente I. Comparison of anterior chamber depth measurements taken with the Pentacam, Orbscan IIz and IOLMaster in myopic and emmetropic eyes. Acta Ophthalmol. 2009; 87:386–91.
Article22. Reddy AR, Pande MV, Finn P, El-Gogary H. Comparative estimation of anterior chamber depth by ultrasonography, Orbscan II, and IOLMaster. J Cataract Refract Surg. 2004; 30:1268–71.
Article23. Jonna G, Channa P. Updated practical intraocular lens power calculation after refractive surgery. Curr Opin Ophthalmol. 2013; 24:275–80.
Article24. Lee AC, Qazi MA, Pepose JS. Biometry and intraocular lens power calculation. Curr Opin Ophthalmol. 2008; 19:13–7.
Article25. Na JK, Kim MS. The comparison of astigmatic outcomes after cataract surgery of inferior versus superior clear corneal incision. J Korean Ophthalmol Soc. 2014; 55:1470–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Astigmatic Correlation between the Automated Refractometry and Dual Scheimpflug Analyzer in Pseudophakic Eyes
- Internal Lens Signal Measured by Dual Scheimpflug Anterior Segment Analyzer
- Comparison of Toric Intraocular Lens Axis Accuracy between Optical Biometry and Dual Scheimpflug Topography
- Intraocular Lens Power Calculation According to the Difference between Anterior and Total Keratometry Using Scheimpflug Imaging
- Comparison of Intraocular Lens Power Calculation Methods Following Myopic Laser Refractive Surgery: New Options Using a Rotating Scheimpflug Camera