J Korean Ophthalmol Soc.
2016 Apr;57(4):540-545. 10.3341/jkos.2016.57.4.540.
The Change of Severity of Epiblepharon after Induction of Total Intravenous Anesthesia without Muscle Relaxant
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. eyeyang@inje.ac.kr
- 2Therapeutics Center for Ocular Neovascular Disease, Inje University Busan Paik Hospital, Busan, Korea.
- 3Department of Anesthesiology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2212785
- DOI: http://doi.org/10.3341/jkos.2016.57.4.540
Abstract
- PURPOSE
To investigate the changes of epiblepharon by evaluating the severity of epiblepharon before and after induction of general anesthesia (GA) with a muscle relaxant and total intravenous anesthesia (TIVA) without a muscle relaxant.
METHODS
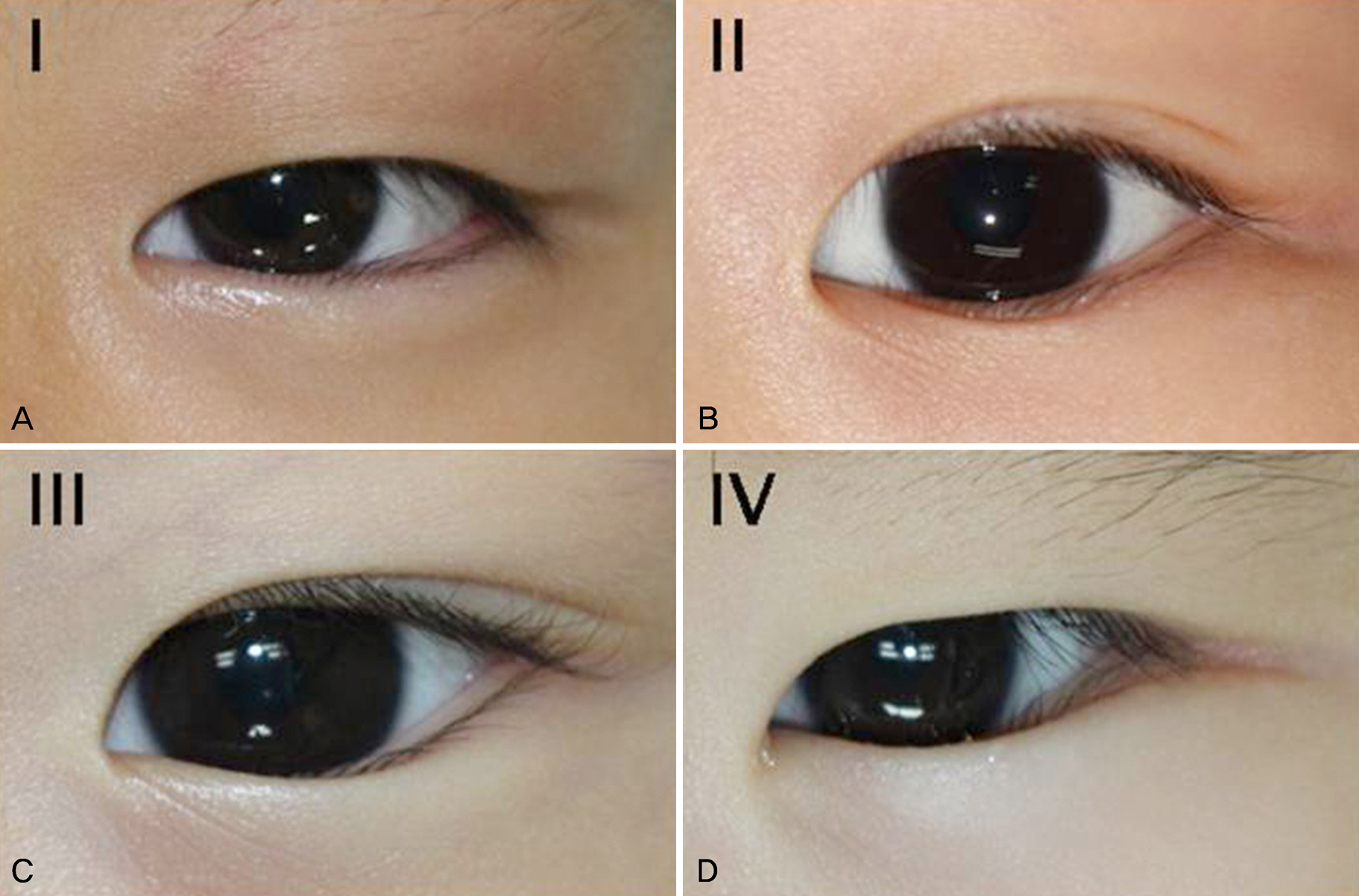
Thirteen pediatric patients (26 eyes) underwent surgery for epiblepharon under GA using a muscle relaxant and 19 pediatric patients (38 eyes) underwent surgery for epiblepharon under TIVA without a muscle relaxant. The severity of epiblepharon in each eye was scored according to skin-fold height (scored 1-4) and area of ciliocorneal touch (scored 1-3) while the patient was in the supine position before induction and after induction of GA.
RESULTS
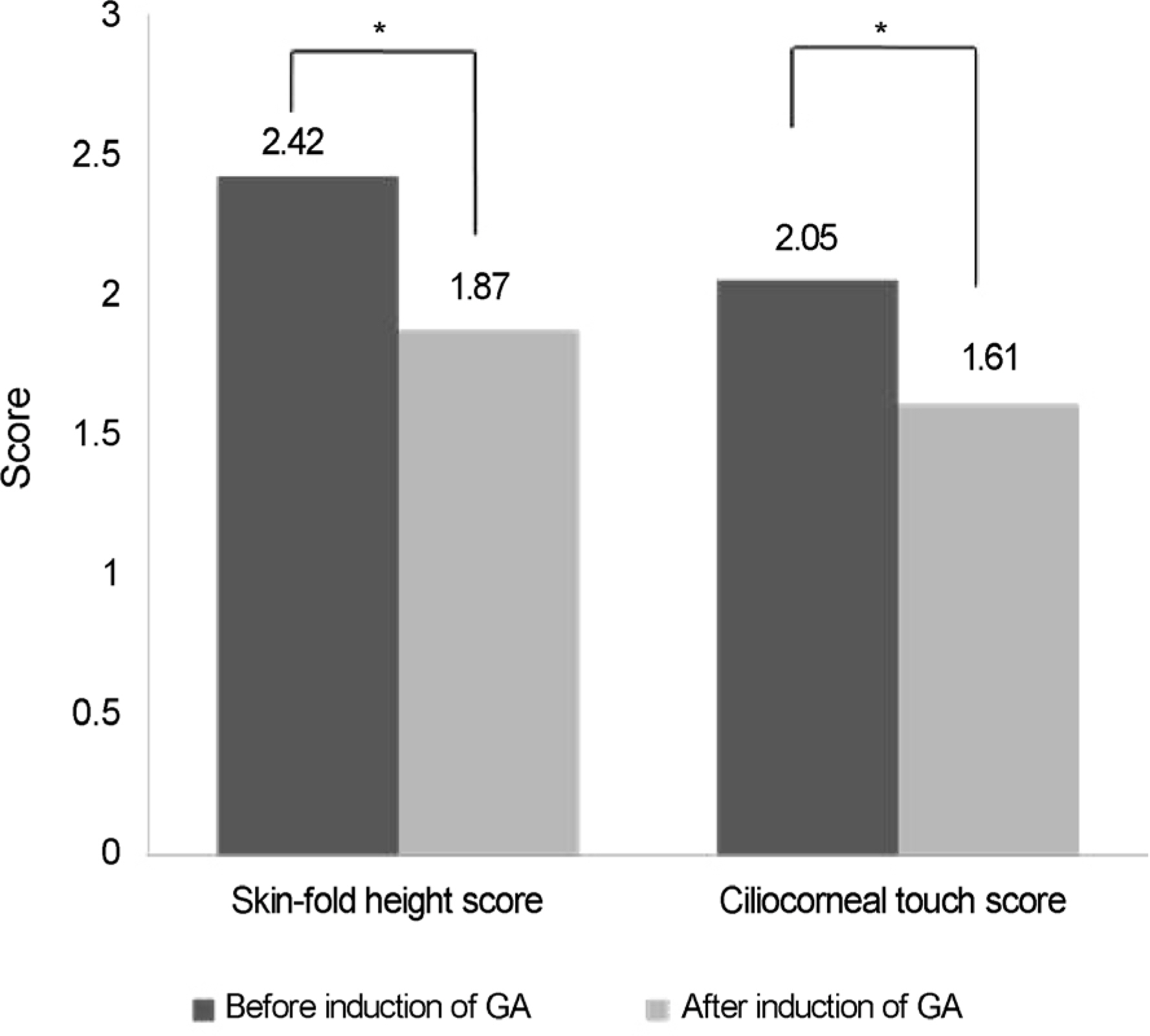
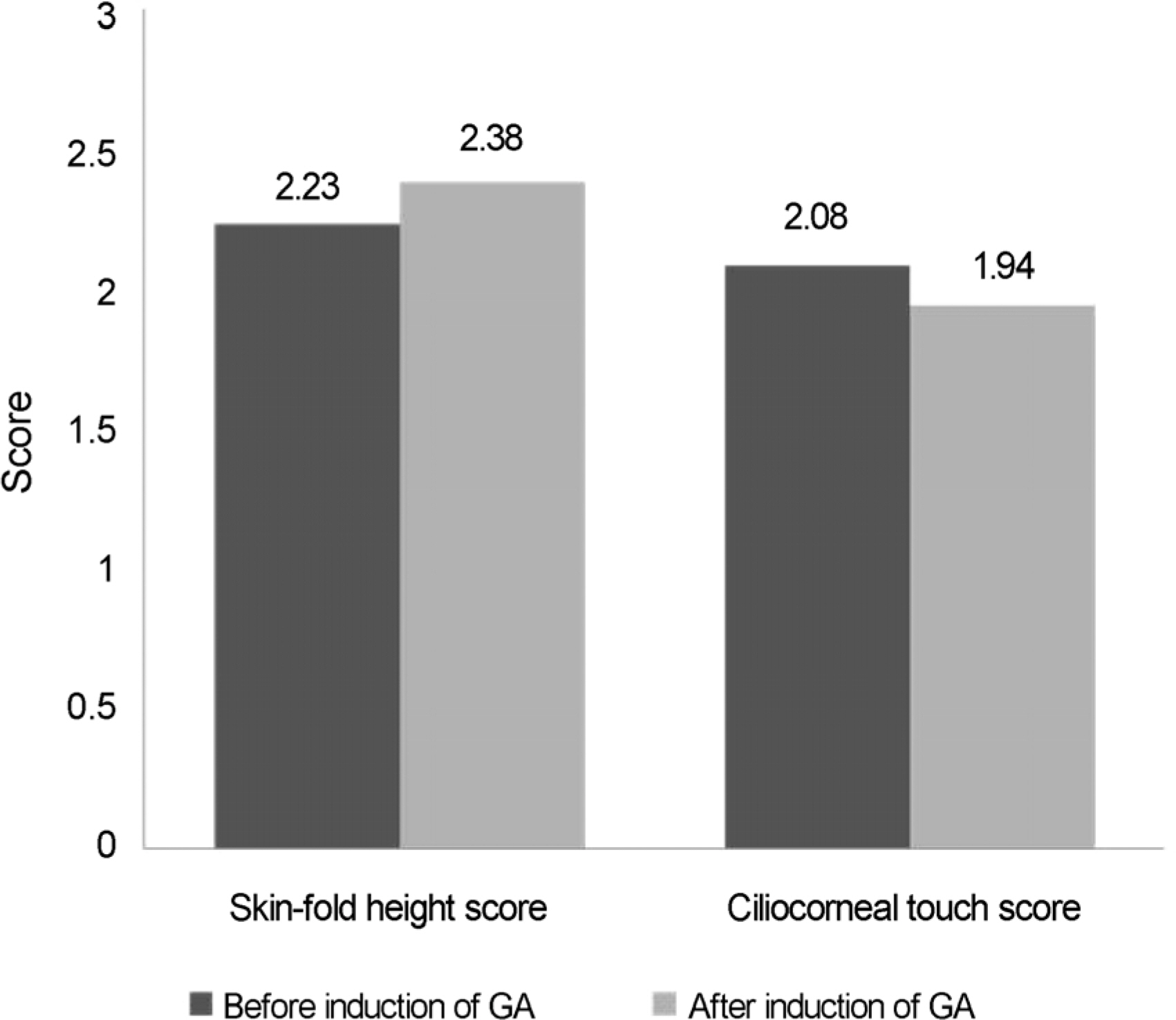
Skin-fold height scores and ciliocorneal touch area scores decreased after induction of GA with a muscle relaxant (skin-fold height score before GA: 2.42 ± 0.86, after GA: 1.87 ± 0.88 p-value < 0.001; ciliocorneal touch area score before GA: 2.05 ± 0.70, after GA: 1.61 ± 0.68, p-value < 0.001). In the TIVA group, skin-fold height scores and ciliocorenal touch area scores were not statistically different before and after GA (skin-fold height score before GA: 2.23 ± 1.18, after GA: 2.38 ± 1.10, p-value = 0.212; ciliocorneal touch area score before GA: 2.06 ± 0.74, after GA: 1.94 ± 0.80, p-value = 0.161).
CONCLUSIONS
The change of epiblepharon severity was significantly reduced by induction of TIVA without a muscle relaxant and there was no recurrence of epiblepharon 3 months after surgery. When using TIVA without a muscle relaxant, the change of epiblepharon severity was reduced and thus, this method can help prevent its undercorrection.
Figure
Reference
-
References
1. Noda S, Hayasaka S, Setogawa T. Epiblepharon with inverted eyelashes in Japanese children. I. Incidence and symptoms. Br J Ophthalmol. 1989; 73:126–7.
Article2. Johnson CC. Epicanthus and epiblepharon. Arch Ophthalmol. 1978; 96:1030–3.
Article3. Levitt JM. Epiblepharon and congenital entropion. Am J Ophthalmol. 1957; 44:112–3.
Article4. Woo KI, Yi K, Kim YD. Surgical correction for lower lid epiblepharon in Asians. Br J Ophthalmol. 2000; 84:1407–10.
Article5. Jordan R. The lower-lid retractors in congenital entropion and epiblepharon. Ophthalmic Surg. 1993; 24:494–6.
Article6. Yang SW, Choi WC, Kim SY. Refractive changes of congenital entropion and epiblepharon on surgical correction. Korean J Ophthalmol. 2001; 15:32–7.
Article7. Quickert MH, Wilkes TD, Dryden RM. Nonincisional correction of epiblepharon and congenital entropion. Arch Ophthalmol. 1983; 101:778–81.
Article8. Kim KS. Neuromuscular block and reversal. J Korean Med Assoc. 2007; 50:1072–80.
Article9. Rhiu S, Yoon JS, Zhao SY, Lee SY. Variations in the degree of epiblepharon with changes in position and induction of general anesthesia. Graefes Arch Clin Exp Ophthalmol. 2013; 251:929–33.
Article10. Khwarg SI, Lee YJ. Epiblepharon of the lower eyelid: classification and association with astigmatism. Korean J Ophthalmol. 1997; 11:111–7.
Article11. Xue FS, Liao X, Tong SY, et al. Dose-response and time-course of the effect of rocuronium bromide during sevoflurane anaesthesia. Anaesthesia. 1998; 53:25–30.
Article12. Lowry DW, Mirakhur RK, McCarthy GJ, et al. Neuromuscular effects of rocuronium during sevoflurane, isoflurane, and intravenous anesthesia. Anesth Analg. 1998; 87:936–40.
Article13. Bock M, Klippel K, Nitsche B, et al. Rocuronium potency and recovery characteristics during steady-state desflurane, sevoflurane, isoflurane or propofol anaesthesia. Br J Anaesth. 2000; 84:43–7.
Article14. Wulf H, Ledowski T, Linstedt U, et al. Neuromuscular blocking effects of rocuronium during desflurane, isoflurane, and sevoflurane anaesthesia. Can J Anaesth. 1998; 45:526–32.
Article15. Harris EA, Lubarsky DA, Candiotti KA. Monitored anesthesia care (MAC) sedation: clinical utility of fospropofol. Ther Clin Risk Manag. 2009; 5:949–59.16. Kurdi MS, Theerth KA, Deva RS. Ketamine: current applications in anesthesia, pain, and critical care. Anesth Essays Res. 2014; 8:283–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in Serum Electrolyte Concentration after Induction of Anesthesia with Intravenous Anesthetics and Nondepolarizing Muscle Relaxant
- Intravenous Anesthesia in Spinal Muscular Atrophy: A case report
- The Use of Total Intravenous Anesthesia Without Muscle Relaxation in Amyotrophic Lateral Sclerosis Patient
- The Influence of a Muscle Relaxant on Bispectral Index during the Propofol Induction of Anesthesia
- Application of Computers in Anesthesiolgy