J Korean Ophthalmol Soc.
2009 Sep;50(9):1423-1426. 10.3341/jkos.2009.50.9.1423.
A Case of Combination Therapy for Subretinal Neovascularization in Bilateral Acquired Parafoveal Telangiectasis
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, College of Medicine, The Catholic University of Korea, Seoul, Korea. wklee@catholic.ac.kr
- KMID: 2212629
- DOI: http://doi.org/10.3341/jkos.2009.50.9.1423
Abstract
- PURPOSE
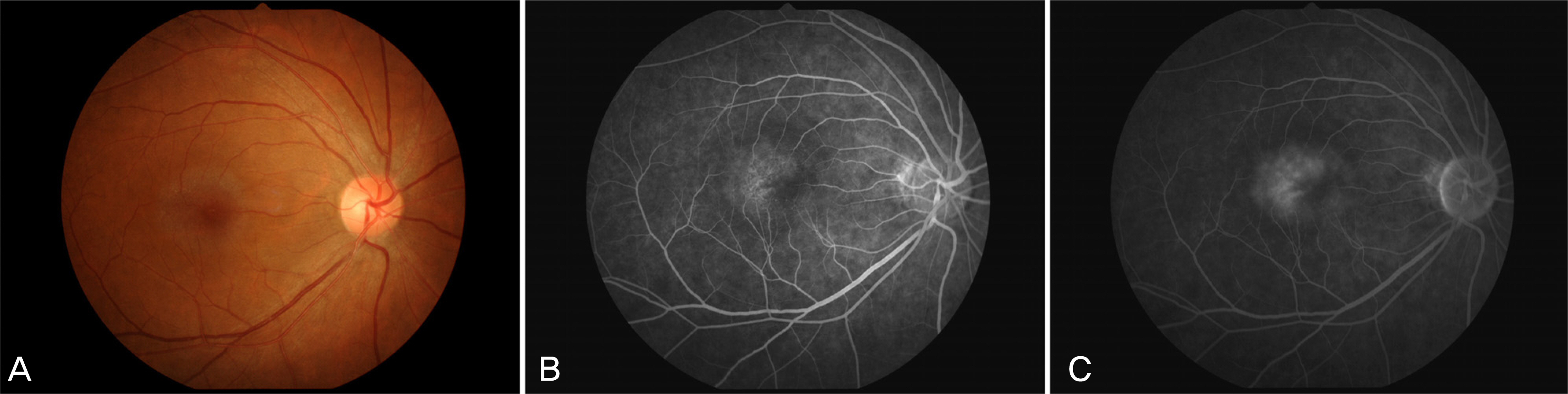
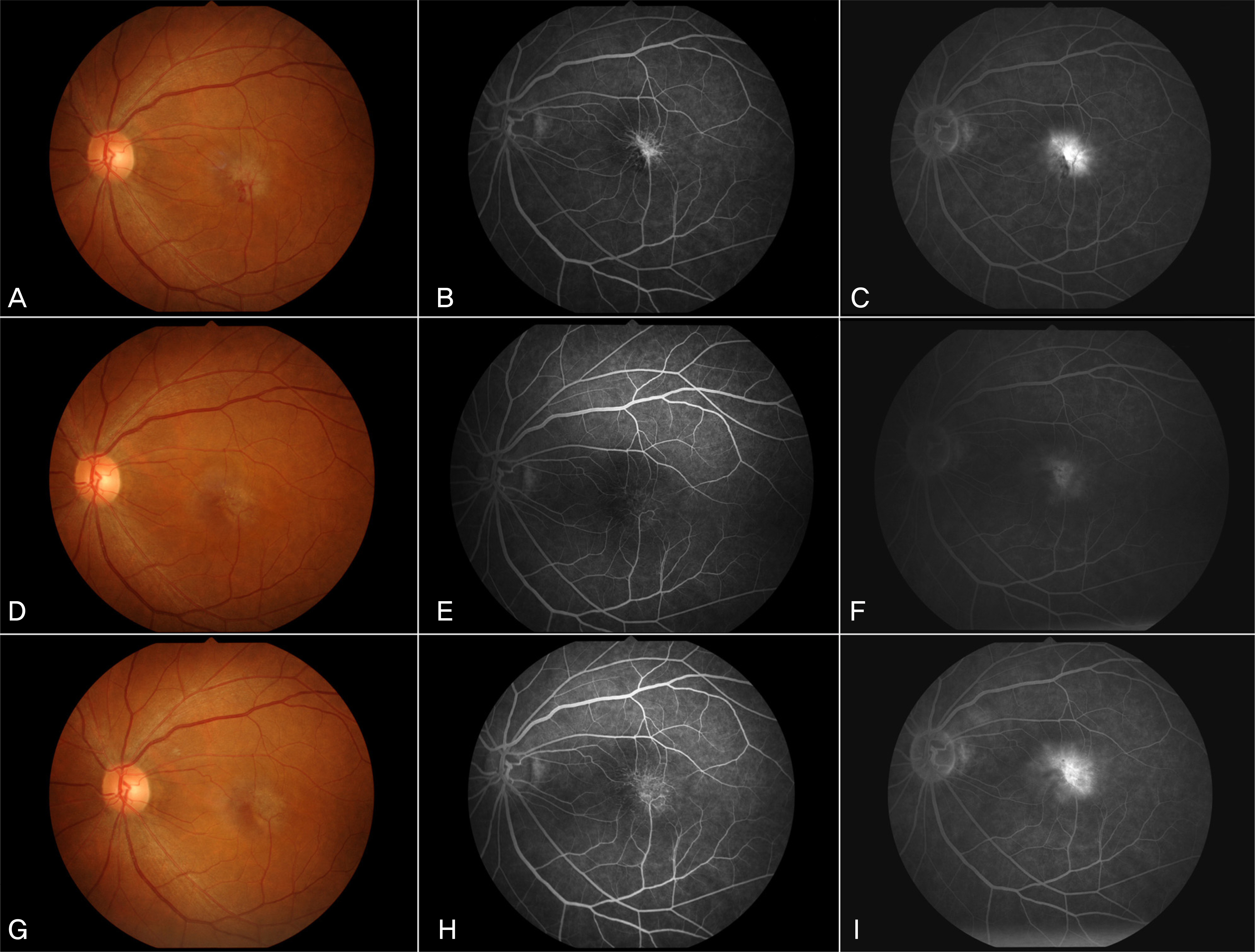
To evaluate the clinical results of a case of subretinal neovascularization (SRN) in bilateral acquired parafoveal telangiectasis, performed combination therapy of intravitreal bevacizumab (1.25 mg/0.05ml) and photodynamic therapy (PDT). CASE SUMMARY: A 46-year-old female presented with a decrease invisual acuity. Her best-corrected visual acuity (BCVA) was 1.0 in the right eye and 0.1 in the left eye. On ophthalmic examination, she was diagnosed with bilateral acquired parafoveal telangiectasis combined with SRN in the left eye. Intravitreal bevacizumab was injected, and then photodynamic therapy was performed 4 days later. Three months after the combination therapy, her BCVA improved to 0.5, a regression of SRN was observed and vascular leakage was markedly decreased. However, her BCVA decreased to 0.1 and SRN recurred 9 months later. CONCLUSIONS: The combined treatment of intravitreal bevacizumab and photodynamic therapy may be used as a selective alternative treatment modality for SRN in bilateral acquired parafoveal telangiectasis, although its effect is short-term.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Bilateral Macular Hole in a Patient with Bilateral Macular Telangiectasia
Suk Jin Kim, Ki Seok Kim
J Korean Ophthalmol Soc. 2013;54(9):1458-1462. doi: 10.3341/jkos.2013.54.9.1458.
Reference
-
References
1. Gass JD, Blodi BA. Idiopathic juxtafoveolar retinal telangiectasis. Update of classification and followup study. Ophthalmology. 1993; 100:1536–46.2. Engelbrecht NE, Aaberg TM Jr, Sung J, Lewis ML. Neovascular membranes associated with idiopathic juxtafoveolar telangiectasis. Arch Ophthalmol. 2002; 120:320–4.
Article3. Hershberger VS, Hutchins RK, Laber PW. Photodynamic therapy with verteporfin for subretinal neovascularization secondary to bilateral idiopathic acquired juxtafoveolar telangiectasis. Ophthalmic Surg Lasers Imaging. 2003; 34:318–20.
Article4. Potter MJ, Szabo SM, Chan EY, Morris AH. Photodynamic therapy of a subretinal neovascular membrane in type 2A idiopathic juxtafoveolar retinal telangiectasis. Am J Ophthalmol. 2002; 133:149–51.
Article5. Snyers B, Verougstraete C, Postelmans L, et al. Photodynamic therapy of subfoveal neovascular membrane in type 2A idiopathic juxtafoveolar retinal telangiectasis. Am J Ophthalmol. 2004; 137:812–9.
Article6. Chang YI, Lee JG, Kim TW, Lee EK. The clinical manifestations and treatment of parafoveal telangiectasis. J Korean Ophthalmol Soc. 2004; 45:576–84.7. Hussain N, Das T, Sumasri K, Ram LS. Bilateral sequential photodynamic therapy for subretinal neovascularization with type 2A parafoveal telangiectasis. Am J Ophthalmol. 2005; 140:333–5.
Article8. Parodi MB, Iacono P, Ravalico G. Subretinal neovascular membrane associated with type 2a idiopathic juxtafoveolar telangiectasis in pseudoxanthoma elasticum. Graefes Arch Clin Exp Ophthalmol. 2007; 245:612–5.
Article9. De Lahitte GD, Cohen SY, Gaudric A. Lack of apparent short-term benefit of photodynamic therapy in bilateral acquired parafoveal telangiectasis without subretinal neovascularization. Am J Ophthalmol. 2004; 138:892–4.
Article10. Smithen LM, Spaide RF. Photodynamic therapy and intravitreal triamcinolone for a subretinal neovascularization in bilateral idiopathic juxtafoveal telangiectasis. Am J Ophthalmol. 2004; 138:884–5.
Article11. Jorge R, Costa RA, Calucci D, Scott IU. Intravitreal bevacizumab (Avastin) associated with the regression of subretinal neovascularization in idiopathic juxtafoveolar retinal telangiectasis. Graefes Arch Clin Exp Ophthalmol. 2007; 245:1045–8.
Article12. Mandal S, Venkatesh P, Abbas Z, et al. Intravitreal bevacizumab (Avastin) for subretinal neovascularization secondary to type 2A idiopathic juxtafoveal telangiectasia. Graefes Arch Clin Exp Ophthalmol. 2007; 245:1825–9.
Article13. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials—TAP report. Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Arch Ophthalmol. 1999; 117:1329–45.14. Moon SJ, Berger AS, Tolentino MJ, Misch DM. Intravitreal bevacizumab for macular edema from idiopathic juxtafoveal retinal telangiectasis. Ophthalmic Surg Lasers Imaging. 2007; 38:164–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Manifestations and Treatments of Parafoveal Telangiectasis
- Subretinal Hemorrhages in High Myopia
- A Case of Bilateral Macular Hole in a Patient with Bilateral Macular Telangiectasia
- A Case of Gronblad-Strandberg Syndrome with Subretinal Neovascularization
- Photodynamic Therapy for Subretinal New Vessels