J Korean Ophthalmol Soc.
2009 Jun;50(6):942-945. 10.3341/jkos.2009.50.6.942.
Ulnar Neuropathy as a Complication of Retinal Detachment Surgery
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University College of Medicine, Seoul, Korea. wismile@unitel.co.kr
- KMID: 2212375
- DOI: http://doi.org/10.3341/jkos.2009.50.6.942
Abstract
-
PURPOSE: To report a case of ulnar neuropathy as an extraocular complication following retinal detachment surgery and face-down positioning.
CASE SUMMARY
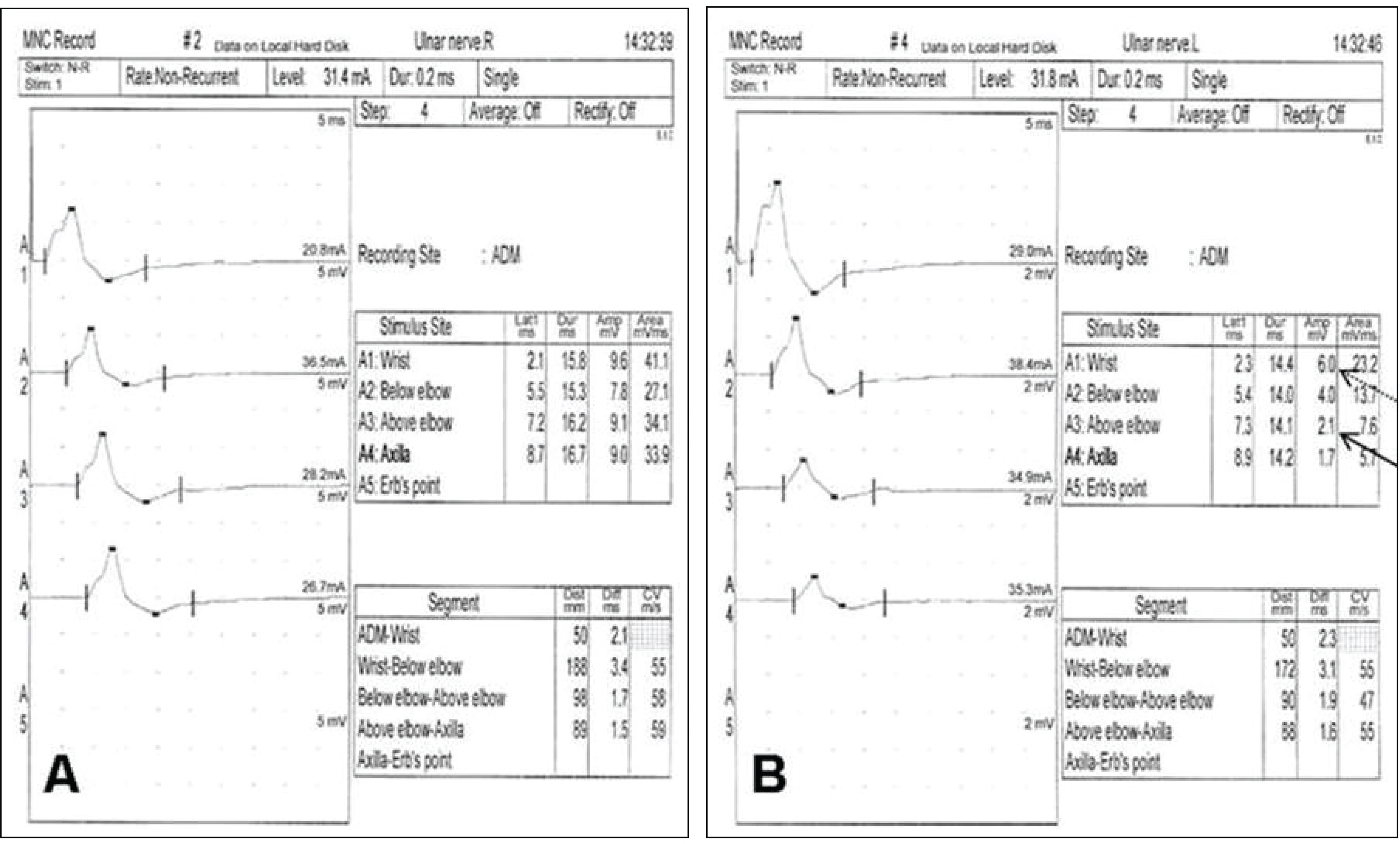
A 65-year-old woman was referred to our hospital with decreased visual acuity in the left eye. Fundus examination revealed a rhegmatogenous retinal detachment not involving the macula in the left eye. A vitrectomy with scleral encircling and 18% SF6 gas tamponade was performed. The patient was instructed to assume a face-down position. After 5 days, the patient reported having paresthesia and numbness of the left 4th and 5th fingers. Neurologic exams were performed and the results indicated ulnar neuropathy. There was no improvement in the neurologic symptoms during the 6-month follow-up.
CONCLUSIONS
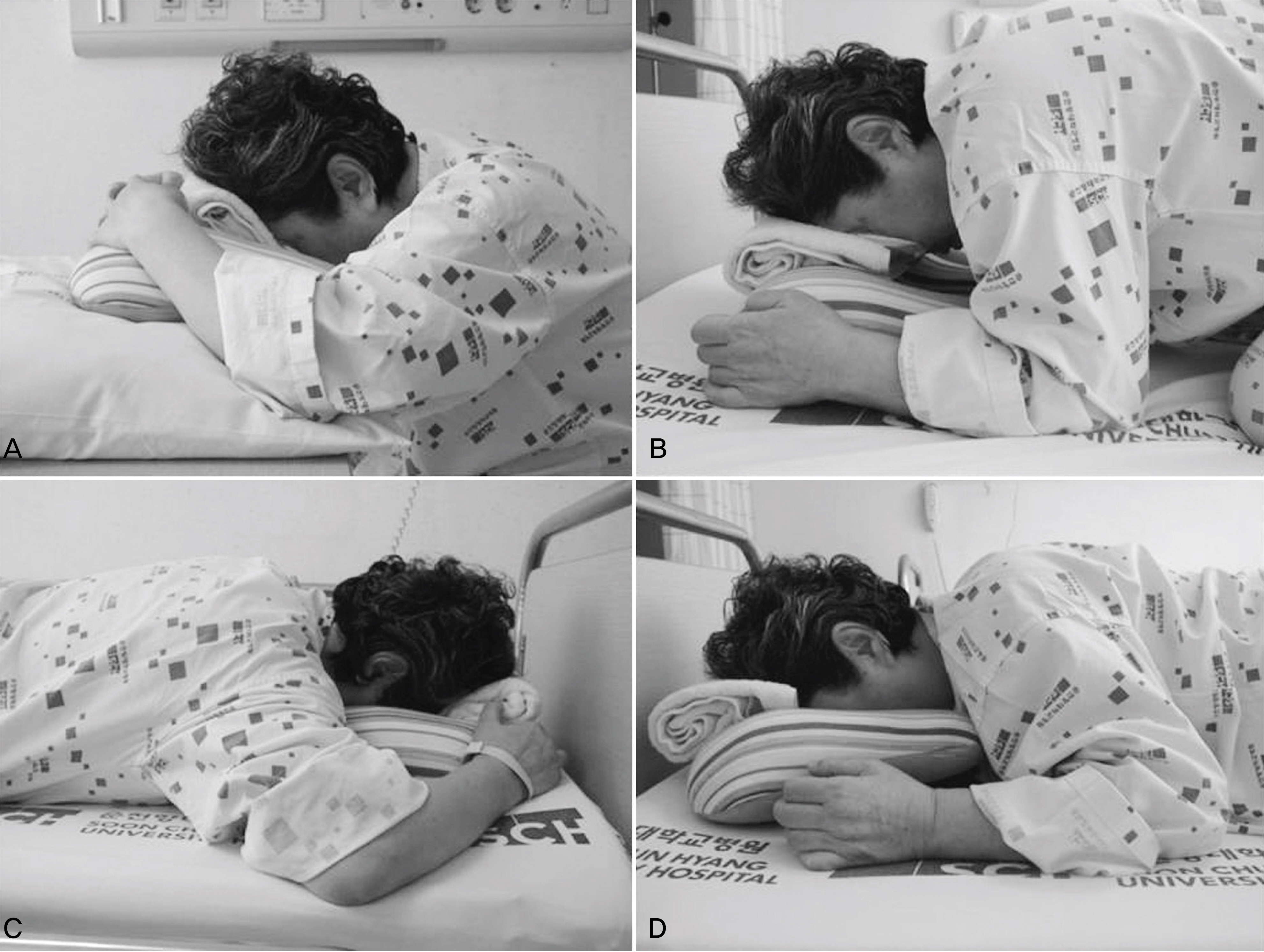
Surgeons performing retinal surgery should caution their patients of ulnar neuropathy when face-down positioning is required. The patients should be instructed to minimize the time spent with their elbows flexed in a stationary position. Additionally, the pressure loaded on the bent elbow should be minimized.
MeSH Terms
Figure
Reference
-
References
1. Holekamp NM, Meredith TA, Landers MB, et al. Ulnar neuropathy as a complication of macular hole surgery. Arch Ophthalmol. 1999; 117:1607–10.
Article2. Salam A, Harrington P, Raj A, Babar A. Bilateral Ulnar nerve palsies: an unusual complication of posturing after macular hole surgery. Eye. 2004; 18:95–7.
Article3. Rabon RJ, Zakov ZN, Meyers SM, Wilbourn AJ. Ulnar nerve mononeuropathies after face-down positioning. Am J Ophthalmol. 1986; 102:125.
Article4. Ciulla TA, Frederick AR Jr, Kelly C, Amrein R. Postvitrectomy positioning complicated by ulnar nerve palsy. Am J Ophthalmol. 1996; 122:739–40.
Article5. Thompson JT, Glaser BM, Sjaarda RN, et al. Effects of intraocular bubble duration in the treatment of macular holes by vitrectomy and transforming growth factor-beta 2. Ophthalmology. 1994; 101:1195–200.
Article6. Thompson JT, Smiddy WE, Glaser BM, et al. Intraocular tamponade duration and success of macular hole surgery. Retina. 1996; 16:373–82.
Article7. Vincent JM, Peyman GA, Ratnakaram R. Bilateral ulnar decubitus as a complication of macular hole surgery. Ophthalmic Surg Lasers Imaging. 2003; 34:485–6.
Article8. Goldbaum MH, McCuen BW, Hanneken AM, et al. Silicone oil tamponade to seal macular holes without position restrictions. Ophthalmology. 1998; 105:2140–7.
Article9. Karia N, Laidlaw A, West J, et al. Macular hole surgery using silicone oil tamponade. Br J Ophthalmol. 2001; 85:1320–3.
Article10. Lai JC, Stinnett SS, McCuen BW. Comparison of silicone oil versus gas tamponade in the treatment of idiopathic full-thickness macular hole. Ophthalmology. 2003; 110:1170–4.
Article11. Tornambe PE, Poliner LS, Grote K. Macular hole surgery without face-down positioning. A pilot study. Retina. 1997; 17:179–85.12. Dhawahir-Scala FE, Maino A, Saha K, et al. To posture or not to posture after macular hole surgery. Retina. 2008; 28:60–5.
Article13. Guillaubey A, Malvitte L, Lafontaine PO, et al. Comparison of face-down and seated position after idiopathic macular hole surgery: a randomized clinical trial. Am J Ophthalmol. 2008; 146:128–34.
Article14. Hilton GF, Das T, Majji AB, Jalali S. Pneumatic retinopexy: principles and practice. Indian J Ophthalmol. 1996; 44:131–43.15. Oh SJ. Clinical electromyography: nerve conduction studies. 3rd ed.Philadelphia: Lippincott Williams & Wilkins;2002. p. 640–1.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ulnar Neuropathy as a Complication of Face-down Positioning after Macular Hole Surgery
- Ulnar Neuropathy Caused by a Schwannoma in the Guyon's Cannal
- A Case of Retinal Detachment with Equatorial Scleral Staphyloma
- A Case of Retinal Detachment with Equatorial Scleral Staphyloma
- Comparision of Clinical Findings between Phakic Retinal and Pseudophakic Retinal Detachment