J Korean Surg Soc.
2011 May;80(5):334-341. 10.4174/jkss.2011.80.5.334.
Lessons learned from 100 initial cases of laparoscopic liver surgery
- Affiliations
-
- 1Department of Surgery, Dong-A University College of Medicine, Busan, Korea. yhkim1@dau.ac.kr
- 2Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea.
- 3Department of Radiology, Dong-A University College of Medicine, Busan, Korea.
- 4Department of Pathology, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2212158
- DOI: http://doi.org/10.4174/jkss.2011.80.5.334
Abstract
- PURPOSE
Laparoscopic liver resection (LLR) is now widely accepted and is being increasingly performed. The present study describes our experience with LLR at a single center over an eight-year period.
METHODS
This retrospective study enrolled 100 patients between October 2002 and February 2010. Forty-six benign lesions and 54 malignant lesions were included. The LLR performed included 58 pure laparoscopy procedures, 18 hand-assisted laparoscopy procedures and 24 hybrid technique procedures.
RESULTS
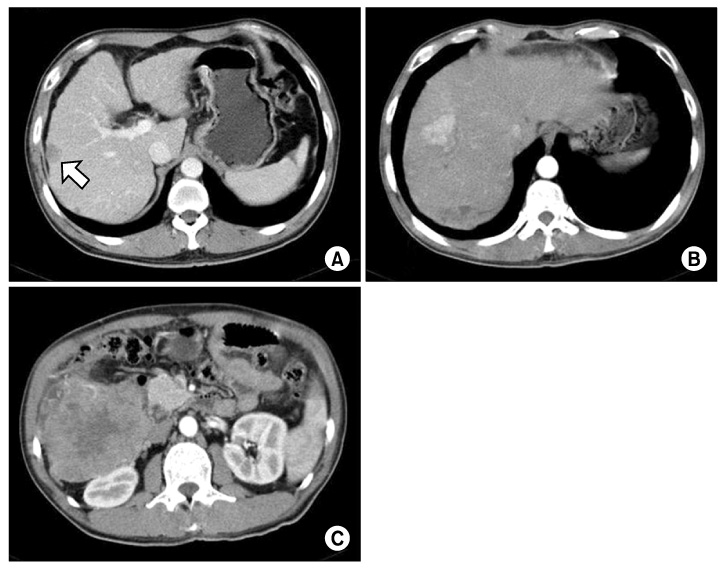
The mean age of the patients was 57 years; among these patients, 31 were over 65 years of age. The mean operation time was 220 minutes. The overall morbidity was 11% and the mortality was zero. Among the 20 patients with simple hepatic cysts, 50% unexpectedly recurred. Among the 41 patients with hepatocellular carcinoma, 21 patients (51%) underwent preoperative radiofrequency ablation therapy or transarterial chemoembolization. During parenchymal-transection, 11 received blood transfusion. The width of the resection margins was under 0.5 cm in 11 cases (27%); 0.5 to 1 cm in 22 cases (54%) and over 1 cm in eight cases (12%). There was no port site seeding, but argon beam coagulation-induced tumor dissemination was observed in two cases. The overall two-year survival rate was 75%.
CONCLUSION
This study suggests that the applications for LLR can be gradually expanded when assuring that the safety and curability of LLR are equivalent to that of open liver resection.
MeSH Terms
Figure
Reference
-
1. Vibert E, Perniceni T, Levard H, Denet C, Shahri NK, Gayet B. Laparoscopic liver resection. Br J Surg. 2006. 93:67–72.2. Otsuka Y, Tsuchiya M, Maeda T, Katagiri T, Isii J, Tamura A, et al. Laparoscopic hepatectomy for liver tumors: proposals for standardization. J Hepatobiliary Pancreat Surg. 2009. 16:720–725.3. Buell JF, Thomas MT, Rudich S, Marvin M, Nagubandi R, Ravindra KV, et al. Experience with more than 500 minimally invasive hepatic procedures. Ann Surg. 2008. 248:475–486.4. Koffron AJ, Auffenberg G, Kung R, Abecassis M. Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg. 2007. 246:385–392.5. Vigano L, Laurent A, Tayar C, Tomatis M, Ponti A, Cherqui D. The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg. 2009. 250:772–782.6. Bryant R, Laurent A, Tayar C, Cherqui D. Laparoscopic liver resection-understanding its role in current practice: the Henri Mondor Hospital experience. Ann Surg. 2009. 250:103–111.7. Han HS, Cho JY, Yoon YS. Techniques for performing laparoscopic liver resection in various hepatic locations. J Hepatobiliary Pancreat Surg. 2009. 16:427–432.8. Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg. 2009. 250:825–830.9. Kaneko H, Tsuchiya M, Otsuka Y, Yajima S, Minagawa T, Watanabe M, et al. Laparoscopic hepatectomy for hepatocellular carcinoma in cirrhotic patients. J Hepatobiliary Pancreat Surg. 2009. 16:433–438.10. Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009. 250:831–841.11. Koffron A, Geller D, Gamblin TC, Abecassis M. Laparoscopic liver surgery: shifting the management of liver tumors. Hepatology. 2006. 44:1694–1700.12. Mazza OM, Fernandez DL, Pekolj J, Pfaffen G, Sanchez Clariá R, Molmenti EP, et al. Management of nonparasitic hepatic cysts. J Am Coll Surg. 2009. 209:733–739.13. Koffron A, Rao S, Ferrario M, Abecassis M. Intrahepatic biliary cystadenoma: role of cyst fluid analysis and surgical management in the laparoscopic era. Surgery. 2004. 136:926–936.14. Dagher I, O'Rourke N, Geller DA, Cherqui D, Belli G, Gamblin TC, et al. Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg. 2009. 250:856–860.15. Nguyen KT, Laurent A, Dagher I, Geller DA, Steel J, Thomas MT, et al. Minimally invasive liver resection for metastatic colorectal cancer: a multi-institutional, international report of safety, feasibility, and early outcomes. Ann Surg. 2009. 250:842–848.16. Poon RT, Fan ST, Ng IO, Wong J. Significance of resection margin in hepatectomy for hepatocellular carcinoma: a critical reappraisal. Ann Surg. 2000. 231:544–551.17. Cherqui D, Laurent A, Tayar C, Chang S, Van Nhieu JT, Loriau J, et al. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg. 2006. 243:499–506.18. Masuda T, Beppu T, Ishiko T, Horino K, Baba Y, Mizumoto T, et al. Intrahepatic dissemination of hepatocellular carcinoma after local ablation therapy. J Hepatobiliary Pancreat Surg. 2008. 15:589–595.19. Ng KK, Poon RT, Lo CM, Yuen J, Tso WK, Fan ST. Analysis of recurrence pattern and its influence on survival outcome after radiofrequency ablation of hepatocellular carcinoma. J Gastrointest Surg. 2008. 12:183–191.20. Spencer L, Metcalfe MS, Strickland AD, Elsey EJ, Robertson GS, Lloyd DM. Lessons from laparoscopic liver surgery: a nine-year case series. HPB Surg. 2008. 2008:458137.21. Kazaryan AM, Pavlik Marangos I, Rosseland AR, Røsok BI, Mala T, Villanger O, et al. Laparoscopic liver resection for malignant and benign lesions: ten-year Norwegian single-center experience. Arch Surg. 2010. 145:34–40.22. Johnson M, Mannar R, Wu AV. Correlation between blood loss and inferior vena caval pressure during liver resection. Br J Surg. 1998. 85:188–190.23. Smyrniotis V, Kostopanagiotou G, Theodoraki K, Tsantoulas D, Contis JC. The role of central venous pressure and type of vascular control in blood loss during major liver resections. Am J Surg. 2004. 187:398–402.24. Wang WD, Liang LJ, Huang XQ, Yin XY. Low central venous pressure reduces blood loss in hepatectomy. World J Gastroenterol. 2006. 12:935–939.25. Uchiyama K, Ueno M, Ozawa S, Hayami S, Kawai M, Tani M, et al. Half clamping of the infrahepatic inferior vena cava reduces bleeding during a hepatectomy by decreasing the central venous pressure. Langenbecks Arch Surg. 2009. 394:243–247.26. Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005. 241:715–722.27. Tralhão JG, Kayal S, Dagher I, Sanhueza M, Vons C, Franco D. Resection of hepatocellular carcinoma: the effect of surgical margin and blood transfusion on long-term survival. Analysis of 209 consecutive patients. Hepatogastroenterology. 2007. 54:1200–1206.28. Viganò L, Tayar C, Laurent A, Cherqui D. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg. 2009. 16:410–421.29. Ohno T, Kawano K, Yokoyama H, Tahara K, Sasaki A, Aramaki M, et al. Microwave coagulation therapy accelerates growth of cancer in rat liver. J Hepatol. 2002. 36:774–779.30. Ikegami T, Shimada M, Imura S, Nakamura T, Kawahito S, Morine Y, et al. Argon gas embolism in the application of laparoscopic microwave coagulation therapy. J Hepatobiliary Pancreat Surg. 2009. 16:394–398.31. Min SK, Kim JH, Lee SY. Carbon dioxide and argon gas embolism during laparoscopic hepatic resection. Acta Anaesthesiol Scand. 2007. 51:949–953.32. Min BS, Lee KY, Park JK, Kim NK, Lee JT, Min JS. Radiofrequency ablation of hepatic metastasis from colorectal cancer: early experience. J Korean Surg Soc. 2002. 62:145–149.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Top Ten Lessons Learned from Trials in Oligometastatic Cancers
- From eminence to evidence and back to presence: lessons learned from the evolution of scientific information dissemination and the case of KJO
- Implementation and lessons learned from 2 online interprofessional faculty development programs for improving educational practice in the health professions in Chile and the United Kingdom from 2018 to 2021
- Lessons from the Initial Experience of Laparoscopic Liver Resection
- Lessons learned in clinical epidemiology of esophageal adenocarcinoma